Leuprolide Injection Causing Pituitary Apoplexy: A Case Report
Grigoriy Gutin, Daniel Landau, Julie Lorton and Krishna Nalleballe
DOI10.4172/2472-1913.100012
Grigoriy Gutin*, Daniel Landau, Julie Lorton and Krishna Nalleballe
Montefiore Medical Center, Albert Einstein School of Medicine, Bronx, NY, USA
- *Corresponding Author:
- Grigoriy Gutin
M.D, Ph.D, Montefiore Medical Center
Albert Einstein School Of Medicine, Bronx, NY, USA
Tel: +44 (0)1784 414229
E-mail: ggutin@montefiore.org
Received date: February 24, 2016; Accepted date: April 08, 2016; Published date: April 18, 2016
Citation: Gutin G, Landau D, Lorton J, et al. Leuprolide Injection Causing Pituitary Apoplexy: A Case Report. J Headache Pain Manag. 2016, 1:2.
Copyright: © 2016 Gutin G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
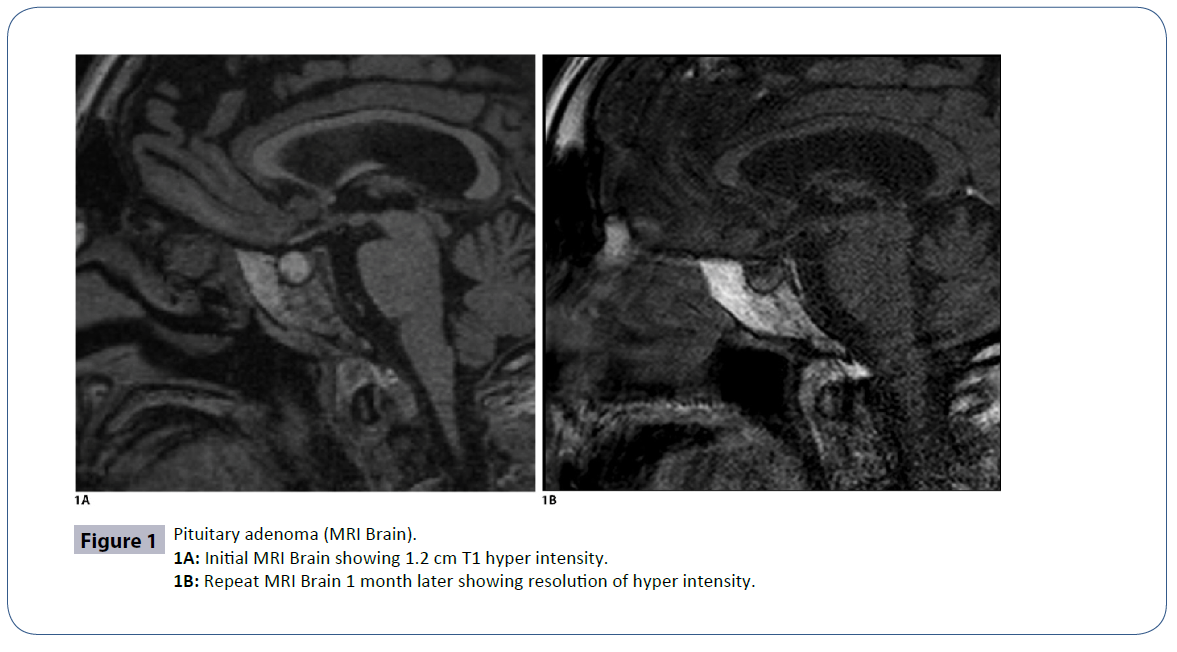
There is growing evidence to support occurrence of pituitary apoplexy following administration of gonadotropin releasing hormone (GnRH) agonists in patients with gonadotropin-secreting pituitary adenomas. We report a case of pituitary apoplexy after depot administration of the GnRH agonist leuprolide. The patient is a 78 year-old man with Gleeson 7, non-invasive prostate cancer who was treated with his first dose of leuprolide two days prior to presentation. He developed a severe headache four hours after leuprolide administration. Non-contrast Magnetic Resonance Imaging (MRI) brain showed a 1.2 cm T1 hyper intensity in the anterior pituitary, likely representing a hemorrhagic adenoma or cyst. 1 month later his repeat MRI of the brain showed resolution of the hemorrhage, as well as a 3 mm lesion within the pituitary thought to be a micro adenoma. What is unique in our case is the mild degree of symptoms manifested by intractable headaches with normal vision and cranial nerve examination, requiring no surgical intervention. There may be a correlation with the size of the adenoma and the severity of disease burden caused by the apoplexy.
Keywords
Leuprolide injection; Pituitary apoplexy; Pituitary macroadenoma
Introduction
Gonadotropin-releasing hormone agonist injections are a standard of treatment for both locally advanced and metastatic prostate cancer [1]. GnRH agonists are synthetic proteins, which interact with the GnRH receptor. Initially they cause a rise in levels of Follicle Stimulating Hormone (FSH), Luteinizing Hormone (LH), and testosterone, which subsequently lead to down regulation of the GnRH receptor; after about one week, testosterone levels decrease to castrate levels [1]. Leuprolide, a synthetic GnRH agonist, has been shown in a number of case reports to be responsible for pituitary apoplexy after administration to patients with a preexisting GnRH-secreting pituitary adenoma [2- 6]. Adding to this literature, we present a case report of a patient who developed pituitary apoplexy after leuprolide administration for treatment of prostate cancer.
Case Report
A 78 year old man with recently diagnosed prostate cancer (Gleeson 7, non-invasive) saw his urologist two days prior to presentation. He was given his first ever-monthly depot injection of the GnRH-analog leuprolide as well as being started on bicalutimide for treatment of his cancer. 4 h after the leuprolide administration he developed a severe headache, described as a pressure-like pain, 7 out of 10, intensity. He denied photophobia, nausea, diplopia, blurry vision, or weakness. He presented to our hospital 2 days later for treatment of the unremitting headache. Other past medical history includes type II diabetes and hypertension. His vital signs were all within normal limits. His exam including the neurological exam was unremarkable. Non-contrast MRI of the brain revealed 1.2 cm T1 hyper intensity of the anterior sella (Figure 1A), which may represent a hemorrhagic adenoma or a cyst.
Initial endocrine labs
| Hormone | Level (Normal Range) | Units |
|---|---|---|
| Thyroid Stimulating Hormone (TSH) | 1.54 (0.400-4.60) | uU/mL |
| LH | 10.7 (0.80-7.60) | mIU/mL |
| Cortisol | 7.1 (5.0-25.0) | ug/dL |
| Prolactin | 19.3 (4.1-15.1) | ng/mL |
| FSH | 2.9 (0.7-11.1) | mIU/mL |
| Growth Hormone | 0.1 (<=7.1) | ng/mL |
| Testosterone | 425 (<1000) | ng/dL |
| Adrenocorticotropic Hormone (ACTH) | 41 (6-50) | pg/mL |
Pituitary axis labs were mostly normal with the exception of mildly elevated prolactin and LH. LH normalized to 5.50 mIU/mL after 2 days and prolactin normalized to 6.7ng/mL after 1 month. His headache resolved after being treated with metoclopramide, ketorolac, and acetaminophen. He did not develop any complications during his hospitalization and did not require surgical intervention. One month after his discharge, he followed up in the endocrine clinic; on his repeat MRI of the brain (this time with gadolinium) (Figure 1B), the previously seen pituitary hyper intensity was gone. The pituitary gland is not enlarged, the stalk is midline, and there is a non-enhancing 3 mm cyst of the left lobe of the pituitary, which may represent a micro adenoma or a small cyst. He is scheduled for a repeat MRI of the brain in one year (Figures 1A and 1B).
Discussion
Leuprolide injections for the treatment of prostate cancer have been utilized for over twenty years. Multiple prior case reports have described the phenomenon of post-leuprolide pituitary apoplexy in patients with underlying pituitary adenomas [2, 5, 6]. In the majority of prior case reports of GnRH agonist-induced pituitary hemorrhage (including leuprolide), the affected patients had more severe presentations including visual deficits, cranial nerve pathologies and altered consciousness [2, 3, 6, 7]. In a review by Guerra et al. from 2010 the majority of pituitary adenomas were large, with average volume 8.8 cm and majority of them showed extension beyond the sella [4]. In patients who underwent pituitary resection as a result of the event and in whom pathology of the underlying adenoma was confirmed, all patients were found to have gonadotroph adenomas, the majority nonfunctional [4].
It is not completely clear of the exact mechanism that leads to the apoplexy. One theory is that it can be due to an acute increase in the blood inflow to the otherwise silent pituitary adenoma, which causes apoplexy [7]. Another possibility is that GnRH agonists cause an increase in the metabolic activity of pituitary adenoma, which causes rapid increase in its volume causing mass effect on surrounding structures which leads to apoplexy [2, 5, 6]. In our case the apoplexy did not cause significant neurological deficits. The only complain of the patient was severe unremitting headache, which improved with treatment. We hypothesize that mild clinical symptoms in part have to be attributed to the size of the pituitary adenoma. In our case, patient was found to have a micro adenoma on MRI. Its mild presentation, benign course and fast resolution without any long-lasting neurological deficits in our case, can be partially attributed to the small size of the pituitary adenoma. As our patient did not undergo pituitary resection the underlying adenoma pathology cannot be confirmed but, in light of normal pituitary hormone profile and the occurrence of post-leuprolide apoplexy, the underlying lesion was most likely a nonfunctional gonadotroph micro adenoma.
Conclusion
Our patient’s benign course in the setting of a relatively small pituitary lesion suggests that the size of the underlying pituitary adenoma may determine the severity of presentation. Our case contributes to the growing pool of evidence suggesting that on rare occasions, leuprolide can cause pituitary apoplexy in predisposed individuals. It is not practical to screen all patients with brain imaging prior to leuprolide administration to decrease the incidence of this very rare complication; however providers should maintain a high index of suspicion for pituitary apoplexy in patients presenting with headache along with other neurologic symptoms following leuprolide therapy.
References
- Van Poppel H, Klotz L (2012) Gonadotropin-releasing hormone: an update review of the antagonists versus agonists. Int J Urol 19: 594-601.
- Engel G, Huston M, Oshima S, Beck C, Harsh G, et al. (2003) Pituitary apoplexy after leuprolide injection for ovum donation. J Adolesc Health 32: 89-93.
- Ito Y (2011) Unexpected enlargement of clinically silent pituitary gonadotroph adenoma induced by goserelin acetate given as treatment for prostate cancer. Int J Urol18: 83-84.
- Guerra Y, Lacuesta E, Marquez F, Raksin PB, Utset M, et al. (2010) Apoplexy in non-functioning pituitary adenoma after one dose of leuprolide as treatment for prostate cancer. Pituitary 13: 54-59.
- Massoud W, Paparel P, Lopez JG, Perrin P, Daumont M, et al. (2006) Discovery of a pituitary adenoma following a gonadotropin-releasing hormone agonist in a patient with prostate cancer. Int J Urol 13: 303-304.
- Sasagawa Y, Tachibana O, Nakagawa A, Koya D, Iizuka H (2015) Pituitary apoplexy following gonadotropin-releasing hormone agonist administration with gonadotropin-secreting pituitary adenoma. J ClinNeurosci 22: 601-603.
- Sinnadurai M, Cherukuri RK, Moses RG, Nasser E (2010) Delayed pituitary apoplexy in-patient with advanced prostate cancer treated with gonadotropin-releasing hormone agonists. J ClinNeurosci17: 1201-1203.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences