Neuroimaging in Headache Disorders
MV Francis
DOI10.4172/2472-1913.100034
Francis MV*
Headache and Neuro Ophthalmology Services, Teresa Eye and Migraine Centre, Cherthala, Alleppey, Kerala, India
- *Corresponding Author:
- MV Francis
Headache and Neuro Ophthalmology Services
Teresa Eye and Migraine Centre
Cherthala, Alleppey, Kerala, India
Tel: 91-9249935280
E-mail: mvfrancis@rediffmail.com
Received Date: October 31, 2016; Accepted Date: January 30, 2017; Published Date: February 10, 2017
Citation: Francis MV. Neuroimaging in Headache Disorders. J Headache Pain Manag. 2017, 2:1. doi: 10.4172/2472-1913.100034
Copyright: © 2017 Francis MV. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
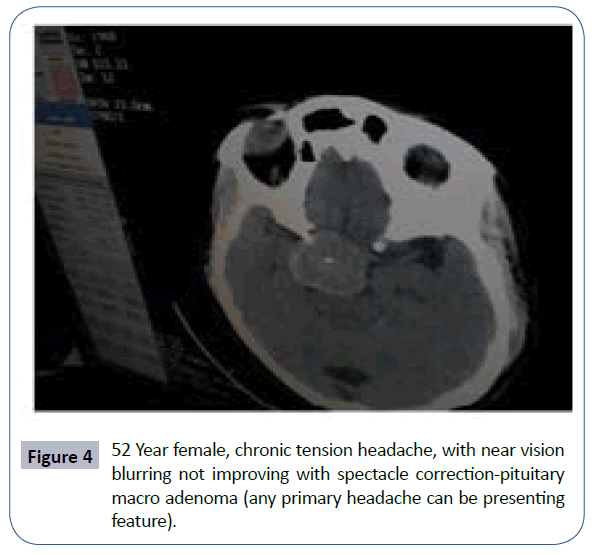
The differential diagnosis for headache is one of the longest in all of medicine, with more than 300 types. Most headaches can be diagnosed correctly without any investigations or testing at all. Utilizing a detailed history mostly based on ICHD 3 Beta diagnostic criteria (14 groups and Appendix/Research criteria) and physical and neurological examinations are all that is necessary in daily practice for diagnosis. In some cases, however diagnostic testing is necessary to distinguish primary headaches like migraine or tension from those secondary headaches that have similar features. Only a small percentage of headache patients require neuro imaging investigations and clinician must make decisions on a case by case basis. In ICHD 3 Beta, comprising 14 groups and an appendix section, no group specifically discusses red flags causing life and vision threatening lesions. Red flags are present in all these groups and it is so scary that ominous disorders like brain tumours, AVMs, Chiasmal lesions, ICA dissection, IIH, CVT etc. can present as primary headache disorders like migraine, tension or trigeminal autonomic cephalalgias. There are some reasons why clinicians frequently order imaging and other tests in headache practice-the quest for diagnostic certainty, it is better to impute disease than to risk overlooking it, busy practice conditions in which tests are ordered as a short cut, high patient expectations, financial incentives, medico legal concerns, the attitude and demands of patients and families and the practice of defensive medicine. The value of any imaging study is determined in large part by the quality of the scanner, the sophistication of the software and the expertise of the person reading the scan. Even the best quality scan may be inadequate if it is the wrong study for the clinical question in hand.
Keywords
Migraine; Cephalalgias; Neuroimaging; Headache
When to Consider Neuroimaging?
Red flag mnemonics
Certain clinical symptoms alert a clinician to consider neuro imaging for patients presenting with acute or recurrent headaches. SNOOP4 (systemic symptoms and secondary risk factors like cancer and HIV/neurological deficit/onset and old age/Symptoms starting with P-papilledma, postural, precipitated by valsalva and progressive) [1-3] is a MNEMONIC which will help physicians to decide about imaging a headache patient. This author has coined a MNEMONIC [4] for red flag signs and symptoms after documenting nearly 500 life and vision threatening intracranial lesions presenting with headaches. This mnemonic is: I W A R N U P lease (I incapacitating, W worst, A abrupt, R recent, N new onset or nocturnal, U unusual headache or symptoms); Please means, signs and symptoms starting with P (Pituitary/Pressure-Eye pressure, both acute and sub-acute angle closure glaucoma, Blood pressure and CSF Pressure-high or low/Papilledema/Posterior/Progressive/Post traumatic/Postural/ Positional/Pattern change/Phacomatosis/Personality changes/ Previous history of headache absent/Precipitated by valsalva/ Prolonged aura/Pounding/Periodic strabismus/Physical exertion/ Pheochromocytoma.
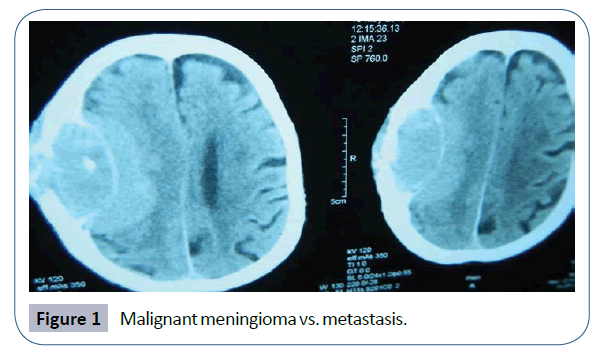
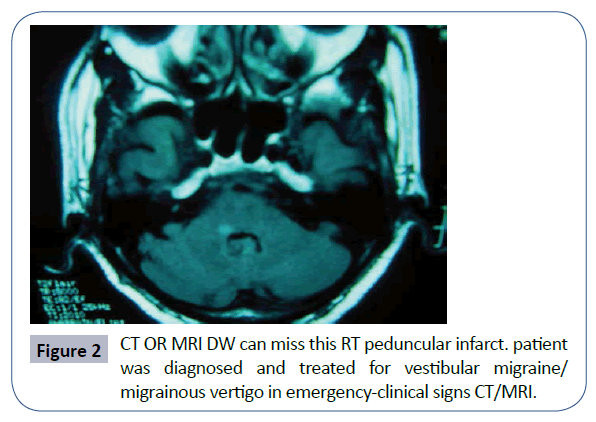
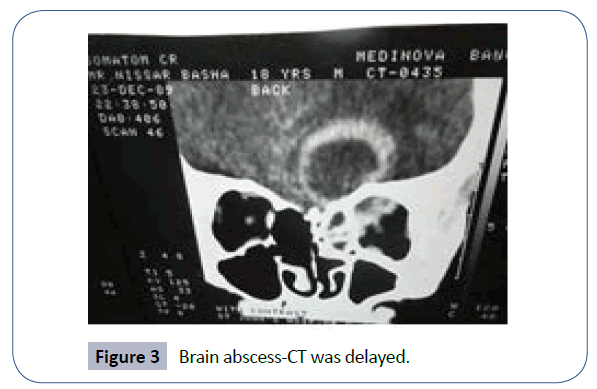
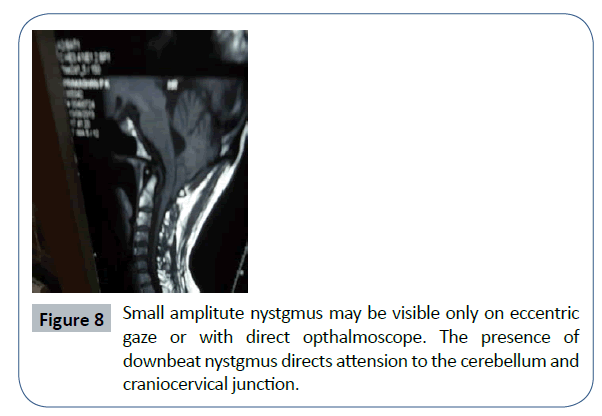
Fever/stiff neck/same side or side locked/focal neurological deficit excepting benign Neuroophthalmological manifestations like Pseudo papilledema, Duanes retraction syndrome, physiological anisocoria or nystagmus, Superior oblique tendon sheath syndrome etc./not responding to treatment/seizures/ Chronic daily headaches too are indications to go for further investigations. The probability of a life-threatening brain lesion increases with these symptoms or signs from 1/1000 to 1500 to 1/10 to 20 (Figures 1-3).
Red Flags in this Patient
CT vs. MRI
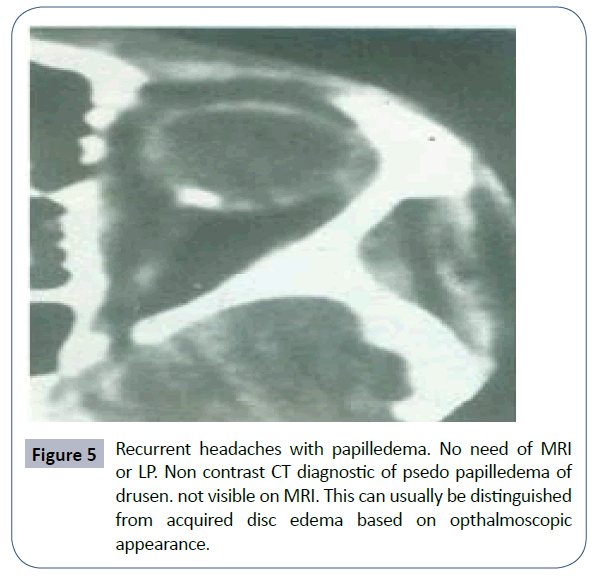
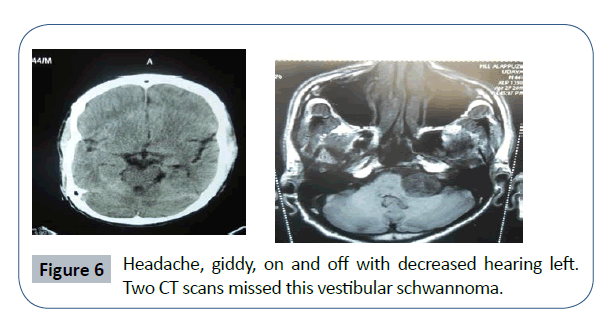
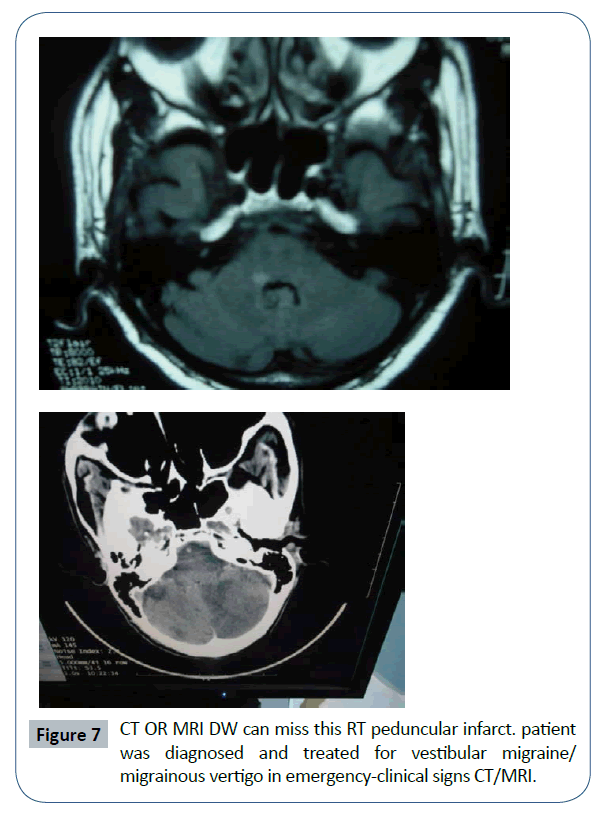
Despite higher cost, MRI is generally preferred to CT for the evaluation of headaches. The yield may vary depending on the field strength (0.2 Tesla to 3 Tesla), the use of paramagnetic contrast, the selection of acquisition sequences and the use of MRA and MRV. However, it may be contraindicated for some patients with aneurysm clip or pace maker. In addition, about 8% of the patients are claustrophobic and about 2% are so claustrophobic that they cannot tolerate the study (Figures 4 and 5). Open MRI with improved image quality may help in this situation. CT will detect most, but not all, abnormalities that can cause headache [5-10]. It is generally preferable to MRI for evaluation of Subarachnoid hemorrhage, after head injury, to detect any bony abnormalities and Hydrocephalus. It is to be remembered always that a number of disorders can miss on routine CT. If CT is normal and symptoms and signs persisting with treatment, think of next imaging modality as CT can miss many brain lesions, especially in the posterior fossa and base of skull (Figures 6-8).
Vascular causes: Saccular aneurysms/AV malformation/SaHGE/ RCVS/Carotid or vertebral dissection/Cerebral infarcts/CVT/Vasculitis/Subdural or epidural hematomas.
Neoplastic: Posterior fossa neoplasms/Meningeal carcinomatosis/ Pituitry tumor and Hemorrhagic Gastroenteritis (HGE).
Cervicomedullary lesions: Chiari malformation, Foramen magnum meningioma.
Infections: Paranasal sinusitis/Meningoencephalitis/Cerebritis and Brain abscess.
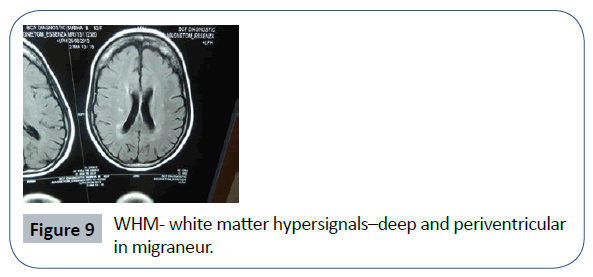
MRI changes in primary headache disorders
White matter abnormalities are seen in 12-46% of migraine patients. They are foci of hyper intensity seen in both proton density and T2 wtd images in the deep and peri ventricular white matter. They are due to interstitial edema, ischemia, peri vascular demyelination or gliosis. One study reported a similar incidence of white matter abnormalities in patients with Tension type headaches and those with migraine. Chronic migraine is associated with number of abnormalities in the CNS. Focal reduction in the cortical gray matter, increased iron deposition in pain related structures, sub cortical white matter lesions and cerebellar infarct like lesions. Recent studies utilizing DT-MRI (diffusion tensor MRI) have shown abnormal white matter properties in several brain regions including body part of corpus callosum in chronic migraineurs. Atrophy of the left hippocampus, right amygdala and larger left lateral ventricular volume also have been documented. Observations from MRA studies are surprising with no extra cranial arterial dilation and only slight intracranial dilation in migraine attacks and Sumatriptan relieved headache and constricted extra cerebral vessels but did not constrict the dilated intra cerebral arteries. In Chronic daily headaches, the following changes have been documented. Increased iron deposition in the peri aqueductal gray, Putamen, Globus pallidus and Red nucleus and also reduction in gray and white matter density and volume depletion in multiple regions of the brain. 3T MRI voxel based morphometry study compared gray matter morphometry of healthy volunteers with that of migraine without aura during and between headache attacks and observed gray matter morphometric changes in the temporo parietal areas over the course of migraine cycle. Brain changes similar to those reported in central vestibular compensation following peripheral vestibular stimulation were noted in Vestibular migraineurs. Wide spread volume decrease in pain and vestibular processing areas including bilateral thalamus and cingulate cortex parallel increasing disease duration and predominant frontal cortex and insula volume decrease as mean headache severity increases, reflecting a strong affective component in Vestibular migraine. In Trigeminal auonomic cephalalgias brain imaging studies show important overlaps between all disorders, notably activation of the posterior hypoythalamic grey. In Hypnic headache, grey matter volume reduction in the hypothalamus has been documented (Figure 9).
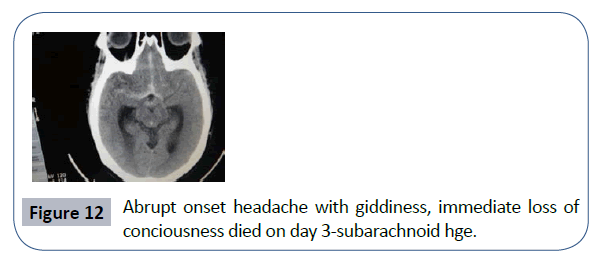
Neuroimaging in the emergency (Thunderclap headaches/Acute severe/new or abrupt onset moderate intensity headaches)
Up to 25% of all the patients presenting to the emergency room with headache of acute onset as their chief complaint would be diagnosed as having SAH. The differentials are-Crash migraine, Cluster headache, associated with vascular disorders like unruptured vascular malformation like aneurysms, Arterial dissections, RCVS, CVA, CVT etc., non-vascular causes like Pituitary apoplexy, IIH, non-cephalic and cephalic infections, colloid cyst of 3rd ventricle, csf hypotension, acute sinusitis and meningitis etc. [11-17].
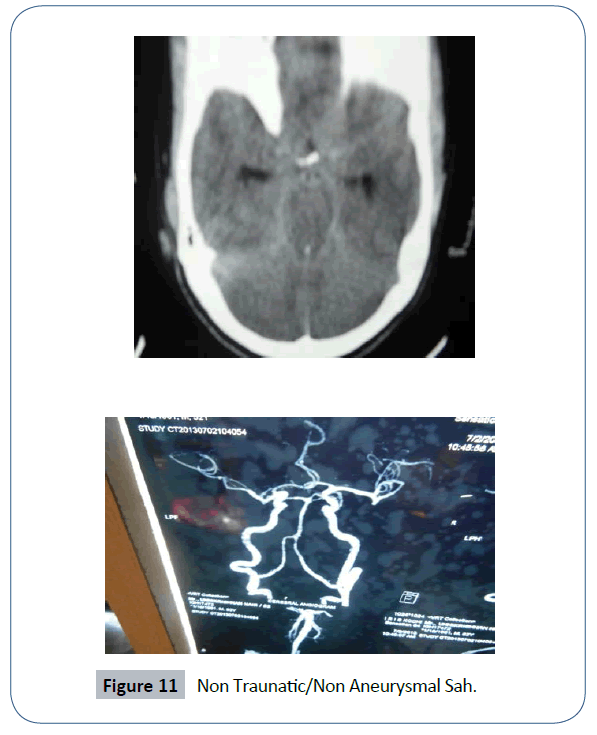
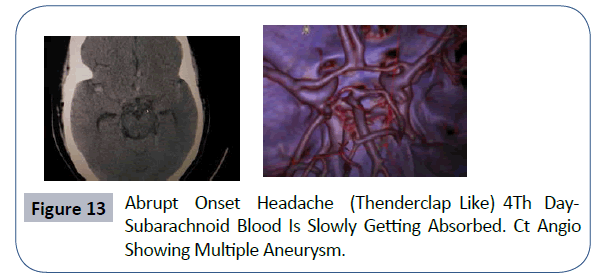
In the acute setting, CT scan without contrast is preferred to MRI for the evaluation of possible subarachnoid hemorrhage because of the wide availability of CT scans, their lower cost and faster scanning time. This has a sensitivity of 98% in the first 12 hours dropping to 93% at 24 hours and 50% at 7 days. According to ICHD 3 Beta and other expert recommendations, if CT results are not diagnostic a Lumbar Puncture is essential. Studies show that for the detection of subarachnoid hemorrhage MRI is almost equal to CT scan in the first 24 hrs and slightly superior in the acute stage up to 72 hrs. From more than 3 to 14 days after the ictus, MRI was definitely superior to CT scan in the identification and delineation of SAH. Once SAH is diagnosed, CTA/MRA/4 vessel angio (catheter/DSA) to be performed to locate the underlying aneurysm. 20% will have multiple aneurysms. Although MRA has not yet replaced cerebral arteriography, it is a useful screening procedure in some cases like when patient refusing 4 vessels or has a thunderclap with normal CT and normal CSF examination. Studies also show that by combining SWI and FLAIR, MRI yields a distinctly higher detection rate for SAH than CT alone, particularly due to their complimentary detection characteristics in different anatomical regions. In one study, CT identified nearly 75%, FLAIR 87% and SWI 88.4% of SAH but combined FLAIR (sensitive for frontal-parietal, temporal-occipital and sylvian cistern SAH) and SWI (particularly sensitive for inter hemispheric and intra ventricular SAH) identified 100%.
RCVS (Reversible Cerebral Vasoconstriction Syndrome) with at least one trivial trigger reported by 80% of patients (emotion, sexual activity, physical exertion, coughing, sneezing, urinating, bathing, showering, sudden head movement etc.) will show strings and beads appearance in MRA. However, CTA, MRA and even catheter angiography can be normal during the first week after clinical onset. Because of this, some RCVS cases need repeat CT or MR angiography 2-3 weeks after headache onset. MRI will be abnormal in 30-80% of cases, showing various patterns of lesions including intracranial hemorrhages (convexity, subarachnoid, intra cerebral or subdural), infarcts, edema or PRES (posterior reversible encephalopathy syndrome). Recent studies show that HVS (Hyper-intense vessel sign-seen in up to 22% patients) on initial FLAIR MRI is useful for an early diagnosis of RCVS [12].
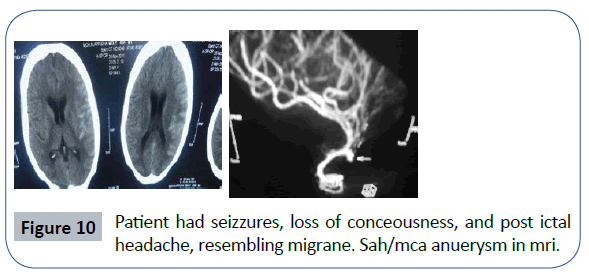
MRA/CTA is extremely sensitive for the detection of cerebral aneurysms, but has not yet achieved 100% accuracy. 92% sensitivity using reformatted images and 98% with source images. The ability of CTA/MRA to detect aneurysms is 100% if the size is larger than 5 mm. If the clinical findings strongly suggest an aneurysm (eg: pupil involved third nerve palsy), a catheter angiogram is necessary, if CTA/MRA is negative (Figures 10-14).
Triggers may be trivial in thunderclap headachesbut don’t forget to image the neck
Trivial triggers like coughing, sneezing, and child birth, athletic activities, painting a ceiling, carrying a heavy load, or riding a roller coaster can precipitate cervical artery dissection. It should be suspected if there is pain in the face, around the eye, in the neck or side of the head (carotid) or back of the head and neck (vertebral), particularly if there has been recent neck injury or manipulation. In carotid artery dissection, there may be an ipsi lateral Horner's syndrome due to involvement of the sympathetic chain, or involvement of the ipsi lateral lower cranial nerves, particularly the hypoglossal. A bruit may be audible on auscultation over the artery. Most cases of Internal carotid dissection can be diagnosed with non-invasive methods, including MRI, MRA, CTA or carotid doppler. The study of choice is an axial T1 or T2 weighted pre-contrast MRI of the head that includes images down to the carotid bifurcation. Dissection appears as a bright crescent shaped signal around the ICA due to hyper-intense signal of methaemoglobin within the vessel wall. Significant narrowing of the lumen, when present, is better documented with MRA or by conventional angiography, and appears as string sign.
Most cases of increased ICP are due to a disease process within the cranial cavity and if the causative lesion is structural, an appropriate scan of the head will reveal it. An important exception to this is a patient with a compressive lesion in the neck producing obstruction of the venous outflow from the head. In such cases the diagnosis may be missed if radiographic studies do not include views of the neck as well as the head.
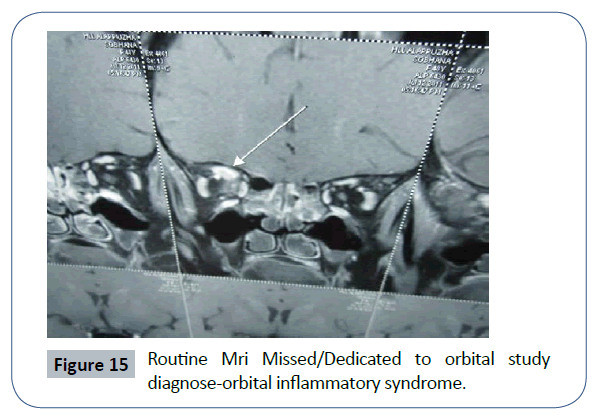
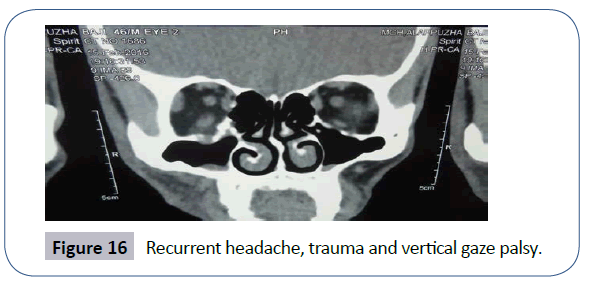
Significance of Contrast MRI
In the evaluation of headache patients with suspected increased ICP (papilledema or symptoms suggestive of raised ICP like transient blurring, diplopia, pulsatile tinnitus, neck, or back pain) CT scanning is usually adequate for excluding a mass lesion and hydrocephalus but is insensitive for the detection of venous sinus thrombosis. CT is also relatively insensitive for the detection of gliomatosis cerebri and meningeal inflammation that may cause increased ICP without ventriculomagaly or mass lesion. Consequently, post contrast MRI has generally been considered a requisite for evaluating for patients with suspected increased ICP. The addition of MRV or CTV is currently recommended to identify those patients with sinus thrombosis. Meningiomas causing headaches are usually isointense on both T1 and T2 weighted images and can be missed if contrast is not given. It is important to be aware of this limitation of non-enhanced scans, particularly in the diagnosis of small tumors. Inclusion of contrast is also important for the detection of orbital inflammation causing periorbital headaches. In evaluating IIH (idiopathic intracranial hypertension), minor abnormalities are seen in MRI like flattening of posterior globe, empty sella, expansion of the perioptic spaces, enhancement of the prelaminar optic nerve, intra ocular protrusion of optic nerve and a small degree of cerebellar tonsillar descent in some patients with chronically increased ICP. Contrast study is also diagnostic in spontaneous CSF hypotension (classically present with postural aggravation with headache occurring immediately or with seconds of assuming an upright position and resolving quickly after lying horizontally), showing dural enhancement (Figures 15 and 16).
Contrast too can miss brain lesions (dedicated imaging is needed)
High resolution MRI with contrast too can miss lesions causing periorbital headaches and holocranial headaches. Two imortant entities are optic nerve sheath meningioma and optic perineuritis (requires fat suppressed, thin section post contrast orbital sequences that include axial and coronal views) and chiasmal region aneurysms (requires dedicated vascular imaging). Infective, non-infectious inflammatory, fistula and neoplastic infiltration may produce subtle signs that go unnoticed even on high grade MRI with contrast.
Pitfalls in MRI Studies
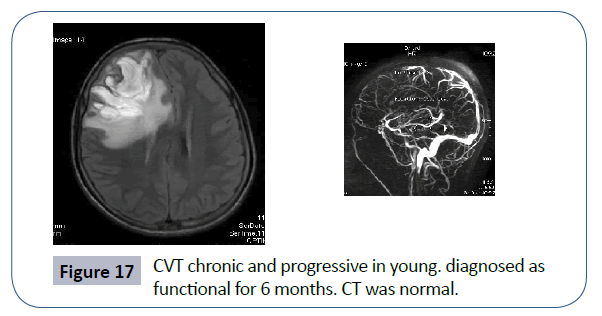
In suspected CVT, relying on MRI alone can be misleading. A falsely negative MRI can occur if the study is performed very early or very late in the course of sinus thrombosis. In the first two or three days following acute thrombosis, the involved sinus is isointense to brain on T1 wtd images and remain hypo intense on T2 wtd images. Later in the course, the sinus may lose its hyperintense signal and regain a more normal appearance, particularly if partial re canalization has occurred. A false positive MRI may occur when venous flow is slowed but not thrombosed. In either case, the additions of venography help clarifying the diagnosis. Post contrast MRV/CTV is highly sensitive for demonstrating absent or decreased venous flow. Similarly, most cases of ICA Dissection can be diagnosed with non-invasive methods, including MRI/MRA or Carotid doppler but evaluation should include MR images of the head and neck (cervical MRI with fat suppression) especially if there is acute onset headache with pain in the face or neck and associated with post ganglionic Horner syndrome (to visualize the area of superior cervical ganglion and carotid bifurcation) (Figure 17)
Indications for DSA/Catheter Angiography, Source and Reformatted Images
If the clinical findings strongly suggest an aneurysm (complete third nerve palsy with pupillary involvement) and if non-invasive tests (MRA) are performed first and are unrevealing. MRA and CTA are extremely sensitive for the detection of cerebral aneurysms; they have not yet achieved 100% accuracy. A recent study comparing MRA techniques to catheter angiography in patients with painful third nerve palsy due to an un ruptured posterior communicating artery aneurysm found a sensitivity of 92% using reformatted images and 98% using source images. Studies using CTA have reported similar high sensitivity for the detection of cerebral aneurysms. The sensitivity depends in part on the size of the aneurysms. The ability of CTA/MRA approaches 100% for aneurysms larger than 5 mm; however, the risk of aneurysmal rupture for less than 5 mm can approach 10%. Headache attributed to Primary or secondary Central Nervous system angitis has no specific features and CTA/MRA are poorly sensitive in detecting them because most cerebral angitis involves the small intracranial vessels which are not well visualized on CTA/ MRA and catheter angiography is necessary in most cases.
Dural carotid cavernous fistula which can present with peri orbital headaches associated with pulsatile tinnitus or ophthalmoplegia, the diagnosis cannot be made solely on the basis of scan findings. MRI and CT do not directly demonstrate a dural fistula but instead reveal signs related to increased orbital venous drainage, providing indirect radiographic evidence for the diagnosis and catheter angiography is the only way to conclusively demonstrate a dural or carotid cavernous fistula and is also necessary for determining the pattern of venous drainage in patients in whom treatment is anticipated.
Imaging Errors and Bony Windows-Both CT and MRI to Be Done
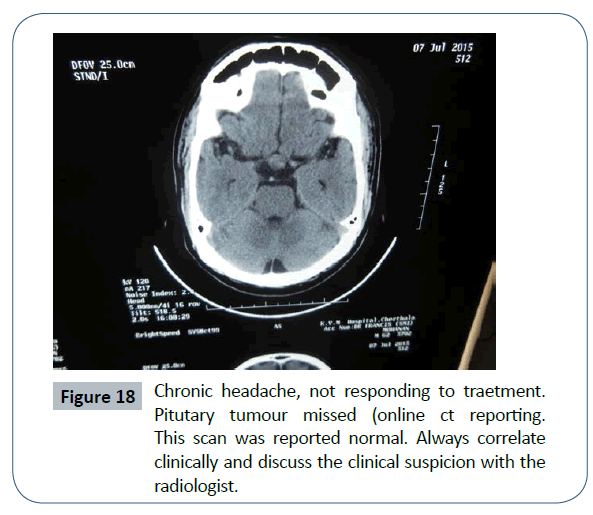
Although a standard head CT is usually the most easily available imaging modality in the emergency, this is less effective than MRI for the detection of Pituitary region lesions especially Pituitary apoplexy. Diagnosing skull base lesions presenting with chronic headaches with or without cranial nerve palsies can be challenging. Standard CT sequences have poor resolution in this region due to signal degradation at soft tissue to bone interfaces. MRI images are not hampered by this limitation, but it do not visualize calcium, so some bony abnormalities may be missed. If skull base tumor is suspected, adequate imaging investigations may require both an MR and CT with bone windows to fully define the site of origin of the lesion and its soft tissue extension (Figure 18).
Persistent Aura or Infarct
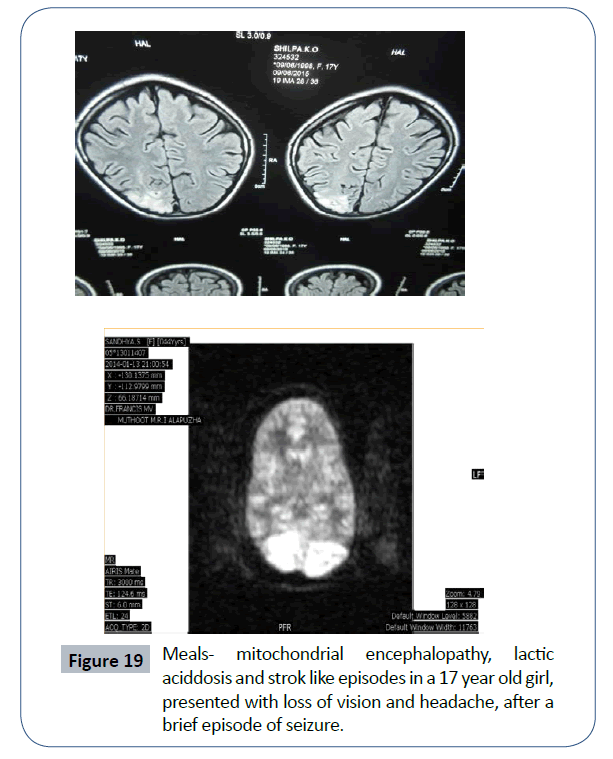
Migraine aura is usually associated with a perfusion deficit not limited to specific/single vascular territory and a moderate increase of Time To Peak (TTP). Hypo perfusion restricted to a single vascular territory with a marked increase in TTP and mean transit time is atypical for migraine with aura and suggestive of acute ischemic stroke. MRA may demonstrate subtle vascular abnormalities like dilated vessels or reduced visualization of peripheral branches in a subset of patients with migraine with aura. Knowledge of these MRI characteristics can be useful to differentiate migraine with aura and ischemic infarction and thus avoid unnecessary thrombolytic treatment in these patients. In Genetic vasculopathies like CADASIL which may present with prolonged aura migraines, MRI T2 wtd imaging will show striking white matter changes. In HaNDL (syndrome of transient headache and neurological deficits with CSF lymphocytosis), episodes of migraine like headaches are accompanied or shortly preceded by the onset of at least one transient neurological deficit which can last more than four hours and routine CT/MRI scans and angiography are normal but ictal brain imaging may show delayed brain perfusion without increased DWI changes, and narrowing of cerebral arteries (Figure 19).
Headache, Cortical Visual Loss, and Negative MRI
Some CNS disorders produce cortical visual loss along with headache but MRI will be normal. They are Migraine with persistent aura, Seizures-ictal and post ictal, Hypoxic ischemic encephalopahy, Non ketotic hyperglycemia and extremely rarely Alzheimers disease and Creutzfeldt-jacob disease. In these entities, the pathologic process was not seen on MRI, not because the lesion was too small or it is overlooked but because these conditions do not generally produce visible changes on routine neuroimaging studies. Functional imaging like fMRI/PET will be of help in some such cases.
Trigeminal autonomic cephalalgias
Many secondary causes of TAC have been reported and neuro imaging to be done emergently. The most common mimicks of Cluster headaches are dissection of carotid or vertebral arteries intracranial aneurysms, tumors or AVM s, cervical cord lesion like meningioma and infarctions. Secondary causes of Paroxysmal hemicrania are circle of willis aneurysms, AVMs, cerebrovascular accidents, collagen vascular disease, tumor of the frontal lobe and sells tercica and cavernous sinus region. The most common mimick of SUNCT (Short lasting unilateral neuralgiform headache with conjunctival injection and tearing) is a lesion in the posterior fossa. In many of these cases, the history and examination disclose features that are worrisome for a secondary cause and the response to conventional medication is lacking [18,19].
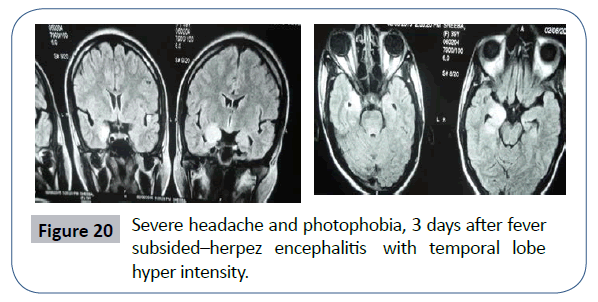
Imaging in meningitis and encephalitis (Group 9, headache attributed to viral meningitis or encephalitis)
Increasing evidence from recent studies suggest that MRI is a powerful tool for the detection of any lesion of the CNS caused by viral infections and helps to initiate timely treatment. In Herpez encephalitis, T2 wtd MRI reveals hyper-intensity corresponding to edematous changes in the temporal lobe, inferior frontal lobes and insula. CT scan may show hypo-density in the temporal lobes but because of the bony artifacts Temporal lobe assessment is less sensitive than MRI. Diagnostic contrast enhancement of the lepto meninges seen in Viral meningitis and diffuse brain edema in encephalitis (Figure 20).
Imaging in group 13-painful cranial neuropathies and other facial pains
According to current evidence, classical trigeminal neuralgias are caused by neurovascular compression, most frequently by superior cerebellar artery and imaging should be done (preferably MRI) to exclude secondary causes and in the majority of patients, to demonstrate neurovascular compression of the trigeminal nerve. MRI of the brain and orbits (with fat suppression) with gadolinium in Optic neuritis and there is a high incidence (90%) of pain with eye movement when there is an orbital segment enhancement and a high probability (70%) of no such pain when there is no such enhancement. When imaging suspected Tolosa hunt syndrome, the clinical features are usually highly localizing but imaging abnormalities are easily overlooked. The contents of the cavernous sinus are usually best assessed by inspection of thin section T1 wtd post contrast views in the coronal plane. In most cases, there is enlargement and increased enhancement of the cavernous sinus. There are no established MRI criteria for the diagnosis of THS but when mild, one must carefully look for expansion of Cavernous sinus on the involved side producing loss of concavity of the lateral wall seen on the normal side. Another method is to do 3D CISS MRI (constructive interference in steady state) to get enhanced pictures of cavernous sinus. In RPON, Recurrent painful ophthalmoplegic neuropathy (previously known as Ophthalmoplegic migraine) gadolinium enhancement or nerve thickening can be demonstrated using MRI [20-22].
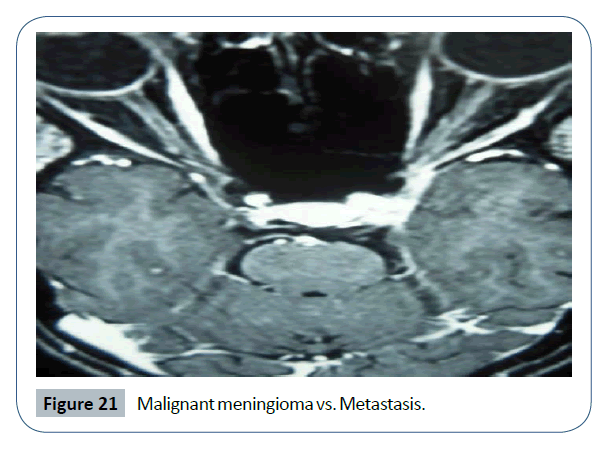
Tolosa hunt syndrome-diplopia and drooping of left lid after 13 days of severe periorbital headache. Thin section post contrast, T1 MRI shows enlargement and enhancement of left cavernous sinus. There may be enhancement of the adjacent dural wall, abnormal soft tissue surrounding and and narrowing the cavernous ICA and extension of this into the orbital apex, sphenoid sinus or floor of the middle cranial fossa. However, it is important to be aware that sometimes even high quality imaging may be normal in THS (Figure 21).
Conclusion
Headache patients, who meet ICHD 3 beta diagnostic criteria for migraine, tension, or TAC, rarely have abnormal neuro imaging findings to explain their headaches. The chance of finding a significant underlying abnormality in patients with a stable headache pattern and a normal neurological examination is extremely rare but if red flags are present neuro imaging must be considered on first consultation or strict follow up is mandatory. In patients, whose headaches could not be adequately classified, the so called atypical headaches, the risk of a significant abnormality was variable and is documented to be as high as 6.7%. Evidence for the trigeminal autonomic cephalalgias harbouring structural lesions is restricted to case reports. A headache questionnaire containing Red flag mnemonic to be given to the patients before examination, so that in a busy practice, decision to image or not can be taken at the earliest. It is also to be remembered that investigation of patients with headache should be balanced against the risk of incidental findings like empty sella syndrome, particularly where investigation is being performed primarily for reassurance.
References
- IHS Classification ICHD-3 Beta (2013) The international classification of headache disorders (ICHD 3 Beta) (3nd edn.) Beta version. Cephalalgia 33: 629-808.
- Duncan CW (2012) Neuroimaging and other investigations in patients presenting with headache. Ann Indian Acad Neurol Aug 15: S23-S32.
- Dodick DW (2003) Clinical Views and Clinical Rules: Primary vs Secondary Headache. Adv Stud Med 3: S550- S555.
- Francis MV (2016) Migraine without aura-towards a new definition. Headache Pain Manag 1: 8.
- Silberstein DS, Lipton RB, Dodick WD (2008) Wolfs headache and other head pain (8th edn.). Oxford Universiy press, London.
- Ravishankar K, Chakravarthy A, Choudhury D, Shukla R, Singh S (2011) Guidelines on the diagnosis and current management of headache and related disorders. Ann Indian Acad Neurol 14: S40-S59.
- Mitchell CS, Osborn RE, Grosskreutz SR (1993) C T in the headache patient: Is routine evaluation necessary? Headache 33: 82-86.
- Hamilton W, Kernick D (2007) Clinical features of primary brain tumors: A case -control study using electronic primary care records. Br J Gen Pract 57: 695-699.
- Kernick DP, Ahmed F, Bahra A, Dowson A, Elrington G, et al. (2008) Imaging patients with suspected brain tumor: Guidance for primary care. Br J Gen Pract 58: 880-885.
- Locker T, Mason S, Rigby A (2004) Headache management–Are we doing enough? An observational study of patients presenting with headache to the emergency department. Emerg Med J 21: 327-332.
- Ravishankar K (2016) Looking at "thunderclap headache" differently? Circa 2016. Ann Indian Acad Neurol 19: 295-301
- Ogawa T, Inugami A, Shimosegawa E (1993) Subarachnoid hemorrhage: evaluation with MR imaging. Radiology 186: 345-351.
- Vermeulen M, Gijn JV (1990) The diagnosis of subarachnoid haemorrhage. J Neurol Neurosurg Psychiat 53: 365- 372.
- Chen SP, Wang SJ (2014) Hyperintense vessels-An early MRI marker of RCVS. Cephalalgia 34: 1053-1061.
- Schwedt TJ, Matharu MS, Dodick DW (2006) Thunderclap headache. Lancet Neuro 5: 621-631.
- Dodick DW (2002) Thunderclap headache. Current Pain Headache Rep 6: 226-232.
- Silvika A, Philbrook B (1995) Clinical and angiographic features of thunderclap headache. Headache 35: 1-6.
- Cittandini E, Mathary MS (2009) Symptomatic trigeminal autonomic cephalalgias. Neurologist 15: 305-312.
- Prakash S, Shah ND, Soni RK (2009) Secondary hemicranias continua: Case reports and literature review. J Neurol Sci 280: 29-34.
- Yousem DM, Atlas SW, Grossman R (1990) MR imaging of Tolosa Hunt Syndrome. AJNR 10: 1181-1184.
- Kline LB, Hoyt WF (2001) The Tolosa Hunt Syndrome. J Neurol Neurosurg Psychiatr 2001: 577-582.
- Francis MV, Nayak US (2002) Ominous peri orbital pain 10th World congress on pain. IASP, San Diego.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences