Peripheral Neurectomy: A Surgical Option for Trigeminal Neuralgia Involving Inferior Alveolar Nerve
Padmanabha Kumar, Shanthi Maleedi and Soma Sekhar Goud
DOI10.4172/2472-1913.100040
Padmanabha Kumar*, Shanthi Maleedi and Soma Sekhar Goud
Mahsa University College, Saujana Putra, Selangor, Malaysia
- *Corresponding Author:
- Padmanabha Kumar
Mahsa University College
Saujana Putra, Selangor, Malaysia
Tel: +603 5102 2200
E-mail: drgpk1@gmail.com
Received Date: May 05, 2017; Accepted Date: July 11, 2017; Published Date: July 25, 2017
Citation: Kumar P, Maleedi S, Goud SS (2017) Peripheral Neurectomy: A Surgical Option for Trigeminal Neuralgia Involving Inferior Alveolar Nerve. J Headache Pain Manag. 2:10 doi: 10.4172/2472-1913.100040
Abstract
Trigeminal neuralgia, a debilitating condition is a commonly diagnosed facial pain with female predominance and with summit of occurrence in the age group of above 40 years. Classic symptoms are excruciating, paroxysmal, shock like pain episodes located in somatosensory distribution of trigeminal nerve. Diagnosis is purely based on typical history and exclusion of secondary causes. Though various treatment options are available, selection of the patient is of utmost important for choosing the appropriate management protocol. No treatment modality is absolutely having recurrence free. Peripheral neurectomy, a minimally invasive and expeditious form of surgical method for the treatment of TN is one of the methods widely practiced even today. Surgical treatment option provides long term pain relief with few complications and also cost effective. We present a case of 62 year-old female patient who has endure peripheral neurectomy of inferior alveolar nerve. No recurrence was noticed in a 3-year follow-up period.
Keywords
Facial pain; Peripheral neurectomy; Trigeminal neuralgia
Introduction
Trigeminal Neuralgia (TN), also known as tic doluoureuxby Nicholas Andre [1] or Fothergill’s disease is a disorder of fifth cranial nerve. The condition was first described by John Fothergill in 1773 Medical Society of London [2]. According to ICHD (international classification of head ache disorders) II criteria (Tables 1A and 1B), classical TN presents as brief episodes of unilateral, recurrent, very severe, electric shock-like and stabbing pain paroxysms, abrupt in onset and termination in the 2nd and or 3rd trigeminal division. Right half [3,4] of the face is more involved than the left. The trigger factors which cause paroxysmal attack of pain [5] are washing, shaving, smoking, talking, or brushing the teeth. High incidence was seen with the age of 40 or older and has predilection for 1.5 times more in women than in men. The etiology [6,7] still remains controversy from no specific reason known as idiopathic to neurovascular conflict in which loop of superior or antero-inferior cerebellar artery contact with trigeminal nerve root resulting in localized demyelination and ectopic triggering of neuronal discharge. Sometimes an inflammatory condition like meningitis, ischemic factors, viral disease [8], drug toxicity [9] and infections of teeth [7] are also contributing factors for TN. Neuropathy can affect any part of the involved nerve from its origin in brainstem to its terminal branches. Even though there are no definitive diagnostic tests to diagnose TN, the diagnosis mainly depends on clinician ability to elucidate about history of pain attacks that are consistent with Sweet’s criteria [10] and exclusion of secondary cases..
| A. Paroxysmal attacks of pain, lasting from a fraction of a second to two minutes, affecting one or more divisions of the trigeminal nerve and fulfilling criteria B and C. |
| B. Pain has atleast one of the following characteristics. • Intense, sharp, superficial or stabbing. • Precipitated from trigger areas or by trigger factors. |
| C. Attacks are stereotyped in the individual patient. |
| D. There is no clinically evident neurological deficit. |
| E. Not attributed to another disorder. |
Table 1A: International classification of headache disorders ICHD criteria for classical Trigeminal Neuralgia.
| A. Parozysmal attacks of pain, lasting from a fraction of a second to two minutes, with or without persistence of aching between paroxysms, affecting one or more divisions of the trigeminal nerve and fulfilling criteria B and C. |
| B. Pain has atleast one of the following characteristics. • Intense, sharp, superficial or stabbing. • Precipitated from trigger areas or by trigger factors. |
| C. Attacks are stereotyped in the individual patient. |
| D. A causative lesion, other than vascular compression, has been demonstrated by special investigations and/or posterior fossa exploration. |
Table 1B: International classification of headache disorders ICHD criteria for symptomatic Trigeminal Neuralgia.
Treatment options of TN includes both conservative medical management and surgical intervention, with each one having its own pros and cons. Factors that determine the mode of the treatment which includes the patient’s age, life expectancy, associated medical conditions and also economic status. Peripheral neurectomy [11] is the oldest of all procedures which consists of minimally invasive surgical avulsion of peripheral part of the involved nerve. The option of peripheral neurectomy on various terminal branches of the trigeminal nerve is still acceptable, more economical as it can be done under local anesthesia, less morbid, cost effective and easily affordable by patients. This case report presents TN involving inferior alveolar nerve.
Case Report
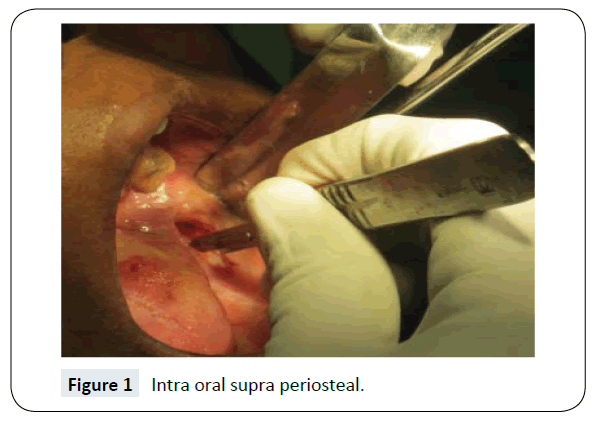
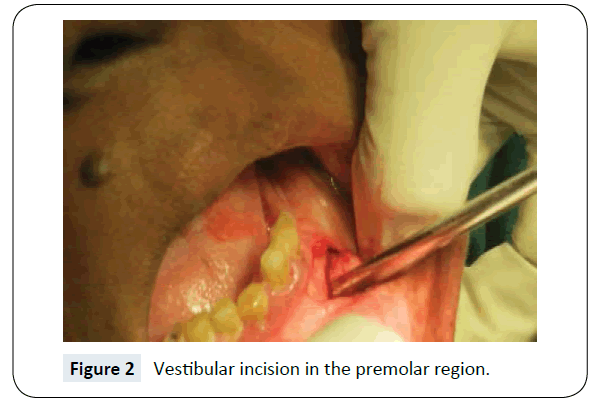
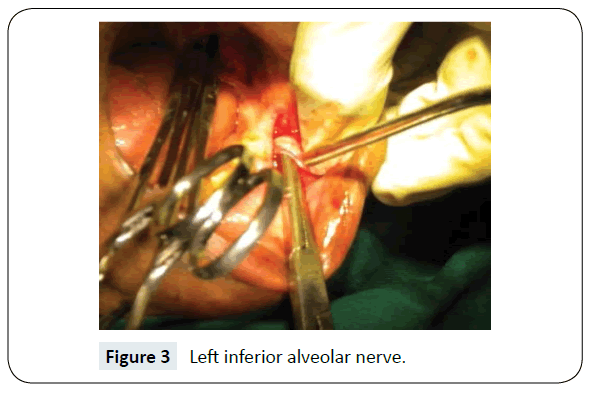
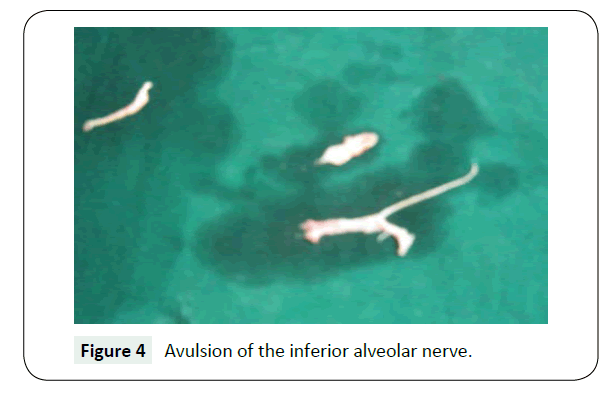
A 62- year-old female patient was referred by general dental practitioner with a history of severe, shock like and throbbing pain in the left V3 region, lasting for few seconds. Aggravating factors are talking, chewing, smiling, with strong breeze and cold water while washing her face. Sleep was disturbed because of pain. Patient described trigger zones to be on left lower pre-molar region. Medical management with drugs like carbamazepine 200 mg (8 hourly) prescribed initially for two weeks then gradually increased up to 600 mg and was advised for 3 months which failed to alleviate her pain. Pre-operative radiographic investigation was done with OPG to rule-out any underlying pathology or any anatomical abnormalities. No abnormality was detected on OPG. The left inferior alveolar nerve was identified according to the site of pain and confirmed by diagnostic block with 2% lignocaine. After thorough examination and confirmation, the patient and her family were explained about the treatment options, its advantages and disadvantages. Informed and written consent obtained, inferior alveolar nerve neurectomy under local anesthesia was planned as patient was reluctance to undergo invasive neurosurgical procedures. High mandibular nerve block by Gow-Gates technique given using 2% lignocaine with 1:2,00,000 adrenaline and Inferior alveolar nerve, lingual nerve, long buccal nerve and mental nerve were blocked. Intra oral supra periosteal dissection done in the retro molar area (Dr. Ginwalla’s incision) (Figure 1). Mandibular foramen was visualized and little above it the neurovascular bundle was identified stretched and held with hemostat. A few mm down another hemostat was used to hold neurovascular bundle. The second vestibular incision in the premolar region was done buccally on the same side (Figure 2). The mental nerve was identified, little stretched and held with another small artery forceps, dissected, ligated and transected. The left inferior alveolar nerve was dissected, ligated and transected between two hemostat just above the mandibular foramen (Figure 3). Avulsion of the inferior alveolar nerve was done from the distal segment from the mental foramen by pulling and rotating the artery forceps at the distal segment area (Figure 4). The mental foramen was closed with bone wax. Layer wise suture done with 3-0 black, non-absorbable silk at both the incision area. Hemostasis was achieved. Routine post-operative antibiotics and anti-inflammatory medications were prescribed for 5 days. Follow up was done to review the patient post-operatively on 2nd, and 7th day to review and rule out pain, infection, and bleeding or suture dehiscence at the surgical sites. Sutures were removed on the 7th post-operative day. Patient was reviewed periodically after 1, 3, 6, 12 and 36 months. In our 36 months follow-up period, patient remains symptom free.
Discussion
Trigeminal nerve with three major divisions is the fifth cranial nerve or CN V, is responsible for sensation of the face including certain motor functions. The ophthalmic and maxillary divisions are purely sensory. The mandibular division has both sensory and motor functions. Diseases which involve the nerve can cause TN or loss of sensory or motor function in the distribution of the nerve. TN involves one or more of the branches of trigeminal nerves, and often causing severe pain.
TN a painful jerking is the most frequently diagnosed form of neuralgia with mean incidence of 4 per 100,000 populations. It usually begins in people over 50 years but can occur at any age at the time of examination [12]. There is a women predominance ranging 1:2 to 2:3. The typical form results in episodes of intense pain, lasting for several seconds to few minutes on one side of the face. Those who are affected experience multiple attacks daily although they are free of pain between attacks; they live in constant fear of recurrences [13]. Diagnosis (Flow Chart 1) is made from a well taken history. The classic clinical pattern which will be inconsistent with sweet’s criteria (Table 2) will lead towards the diagnosis. Sweet’s criteria [10] to diagnose trigeminal neuralgia are: The unilateral pain is paroxysmal, provoked by light touch on the face (trigger zone) which is confined to trigeminal distribution with normal clinical sensory examination. Other differential diagnosis [14] like tooth ache, stomatitis, sinusitis, bursts of head ache, otitis media, paroxysmal hemicranias, acoustic neurilemma, craniofacial/atypical facial pain, post traumatic neuralgia, post herpetic neuralgia, giant cell arteritis. All patients should ideally have MRI scanning or atleast a CT scan. Preoperative localization of compressive vessels at the root entry zone is done by MRI scanning. The diagnosis and management of TN is multi-disciplinary approach with neurologists, oral and maxillofacial surgeons, neurosurgeons.
Flow Chart 1: Diagnostic algorithm for Trigeminal Neuralgia by Scrivani et al. [10].
| • The pain is paroxysmal. • The pain may be provoked by light touch to the face (trigger zones). • The pain is confined to trigeminal distribution. • The pain is unilateral. • The clinical sensory examination is normal. |
Table 2: Sweet diagnostic 5 major criteria for Trigeminal Neuralgia.
Conservative (medical) treatment consists of drug therapy (Table 3). For those who are suffering from refractory to such treatment, other procedures are non-invasive technique like: (a) Peripheral neurectomy, (b) Alcohol injections, (c) Cryotherapy, (d) Selective radio frequency thermo-coagulation. Invasive techniques are: (i) Open micro vascular decompression and (ii) Percutaneous: (a) Radiofrequency rhizotomy, (b) Retrogasserian glycerol rhizotomy, (c) Balloon compression of trigeminal nerve, (d) Stereostatic radiosurgery–gamma knife is advised [12]. Peripheral neurectomy [15] of the peripheral branches of trigeminal nerve is simplest, safest and minimally invasive surgical procedure as reported by many authors. Several studies [16] published the retrospective case series of neurectomies for period of 0-9 years. On an average pain relief of 24-32 months was noticed. Shah et al. [11] evaluated the role of peripheral neurectomies in the treatment of trigeminal neuralgia in modern practice by analyzing 50 patients. 70% of patients had excellent pain relief for a period of 2-5 years and concluded peripheral neurectomy is done for elderly patients. In our case of 3-yearfollow up, no episodes of pain occurred. She remained symptom free with relief of pain.
| Drug | Initial dose | Maintenance dose |
|---|---|---|
| Gabapentin | 300 mg tid | 1800 mg |
| Baclofen | 5 mg bid/tid | 80 mg maximum dose |
| Clonazepam | 0.5 mg tid | 4 mg, maximum 20 mg |
| Lamotrigine | 50 mg qd | 300-500 mg |
| Oxcarbazepine | 300 mg bid | 1200 mgbid |
| Toprimate | 50 mg qd | 200 mg bid |
| Carbamazepine | 100 mg bid | 1200-2400 mg |
Table 3: Drug therapy for Trigeminal Neuralgia.
Conclusion
There is no ideal surgical treatment for TN and case should be selected on the basis of individual’s merits and demerits. Peripheral neurectomy, even though is the oldest technique, is an ideal treatment of choice in those patients who are refractory to medical therapy and patients who cannot offered and indicated for invasive procedures in general anesthesia. It acts by interrupting the flow of a significant number of afferent impulses to central trigeminal apparatus. Newer approaches include physiological inhibition of pain by transcutaneous neural stimulation and even acupuncture, which needs more research on it. Psychological and social support also play key role in the management of chronic illness of TN.
References
- Brown JA, Coursaget C, Preul MC, Sangvai D (1999) Mercury water and cauterizing stones: Nicolas Andre and tic doluoureux. J Neurosurg 90: 977-981.
- Nurmikko TJ, Eldridge PR (2001) Trigeminal neuralgia–pathophysiology, diagnosis and current treatment. Br J Anaesth 87: 117-323.
- Tiffany LM II (1896) Intracranial operations for the cure of facial neuralgia. Ann Surg 24: 575-619.
- Harness DM, Chase PF (1990) Lateralization of chronic facial pain: Fact or fiction. Cranio 8: 339-341.
- Apfelbaum L (1982) Surgical management of disorders of the lower cranial nerves. In: Schmideck HH, Sweet WH (eds.) Operative neurosurgical techniques. New York: Grune and Stratton pp: 1063-1082.
- Joffroy A, Levivier M, Massager N (2001) Trigeminal neuralgia. Pathophysiology and treatment. Acta Neurol Belg 101: 20-25.
- Easton HG (1970) Zooster sine herpete causing acute trigeminal neuralgia. Lancet 37: 1065-1066.
- Baskin DS, Jownseed J, Wilson CB (1981) Isolated hypertrophic neuropathy associated with trigeminal neuralgia. J Neurosurg 55: 987-990.
- Grantham EG, Segerberg LH (1952) An evaluation of palliative surgical procedures in trigeminal neuralgia. J Neurosurg 9: 390-394.
- Scrivani SJ, Mathews ES, Maciewicz RJ (2005) Trigeminal neuralgia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 100: 527-538.
- Shah SA, Khattak A, Shah FA (2008) The role of peripheral neurectomies in the treatment of trigeminal neuralgia in modern practice. Pak Oral Dent J 28: 237-240.
- Bagheri SC, Farhidvash F, Perciaccante VJ (2004) Diagnosis and treatment of patients with trigeminal neuralgia. J Am Dent Assoc 135: 1713-1717.
- Liu JK, Apfelbaum RI (2004) Treatment of trigeminal neuralgia. Neurosurg Clin N Am 15: 319-334.
- Malik NA (2012) Textbook of oral and maxilla-facial surgery (4th edn.). Jaypee Publishers.
- Cerovic R, Juretic M, Gobic MB (2009) Neurectomy of the trigeminal nerve branches: Clinical evaluation of an “obsolete” treatment. J Craniomaxillofac Surg 37: 388-391.
- Quinn JH (1965) Repetitive peripheral neurectomies for neuralgia of second and third divisions of trigeminal nerve. J Oral Surg 23: 600-608.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences