Preictal Symptomatology in Migraines: Diagnostic and Therapeutic Significance
Surya N Gupta, Vikash S Gupta and Gira Borad
DOI10.4172/2472-1913.100007
Surya N Gupta1*, Vikash S Gupta2, Gira Borad3
1Department of Child Neurology, Women’s and Children’s Hospital, Charleston Area Medical Center, Charleston, West Virginia, USA
2Texila American University, Woolford Ave, Georgetown, Guyana, USA
3Department of Child Neurology, Charleston, West Virginia, USA
- *Corresponding Author:
- Surya N Gupta
Associate Professor, Pediatric Neurology, 830 Pennsylvania Ave
Suite 201, Charleston, WV 25302, USA
Tel: +1 304 545 1971
Fax: +1 304 388 6955
E-mail: suryangupta@rediffmail.com
Received date: November 18, 2015; Accepted date: January 28, 2016; Published date: February 08, 2016
Citation: Gupta SN, et al. Preictal Symptomatology in Migraines: Diagnostic and Therapeutic Significance. Headache Pain Manag. 2016, 1:1.
Copyright: © 2016 Gupta SN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Prodrome and aura constitute preictal symptomatology of migraines. The objective of this clinical review is to examine the diagnostic and therapeutic significance of preictal symptomatology in children with migraines. The systemic review of the literature identified a single study in children with migraines. The majority studies were in adults. Based on our search and longitudinal clinical observation, we describe the clinical characteristics of diagnostic and therapeutic significance of preictal symptoms and various types of auras in migraines. Such significance can be substantially increased by including prodromal physical signs in children with migraines. Future studies’ methodology should include physical signs in addition to symptoms and identify the spectrum of the various auras, and relate to their temporal association with ictal and postictal phases of migraines. In addition these clinical parameters should be statistically analyzed.
Keywords
Preictal symptomatology; Prodrome; Aura; Migraine attack profile; Migraine without aura; Migraine with aura; Migraine-related condition; Therapeutic implication
Introduction
Many perceive that they do not have migraine because they do not have headache or an aura. The migraine attack profile is a continuum of three main phases; prodrome, ictal, and postictal. A prodrome is an early symptom or set of symptoms that indicates the onset of a disease. Aura occurs just before the ictal phase. In contrast to seizure, the entire event in migraine lasts hours rather than a few minutes [1]. In the past, “Neglected”, “Anecdotal”, and “Incompletely explored”, are a few words that have been used to describe the status of prodromes in migraine.
The International Classification of headache disorders-3rd Edition, beta version (ICHD-3 beta, 2013) defines prodrome as non-headache symptoms occurring 2–48 hours before the onset of headache or aura. However, the diagnostic criteria for migraine with and without aura do not include prodromal symptoms [2].
When considering a diagnosis of migraine, a full spectrum of migraines such as migraine without aura, migraine with aura, and migraine-related condition should be considered. The first two subtypes of migraine can be diagnosed by obtaining a sequential history of the onset of the very first symptom and following the unfolding symptoms of the migraine attack profile.
The majority of patients with migraine do not have aura, but they do have a prodromal symptom. Almost all patients with migraine related condition have atypical aura and an insignificant history of headache. The status of prodrome in migraine-related condition is unknown. However, this is typically not acknowledged by the patients [3].
Of note: The terms prodrome and premonitory are used interchangeably in migraine. By definition, the premonitory phase unlike prodrome has a very short duration.
Method
Literature search
To identify diagnostic and therapeutic significance of preictal symptomatology in children and adults with common migraine, migraine with or without aura, and migraine-related conditions, we performed a systemic PubMed online search. We used terms preictal sign, preictal symptom, prodromal symptom or sign, premonitory symptom, typical aura, and atypical aura in isolation or in combination.
We supplemented our search with surveillance of electronic tables of contents and by hand searching the bibliographies of pertinent articles. Two authors (SG and GB) read the title and abstract of every identified study and critically appraised the full text of potentially eligible studies.
Studies in which key element of preictal symptomatology or diagnostic and therapeutic significance in migraines could not be extrapolated were excluded from this clinical review.
The results
Table 1 summarizes the studies of prodrome reported in children and adults with migraines [4-11]. Our search reveals no devoted studies to the diagnostic and therapeutic significance of preictal symptomatology in migraines.
| Study Type [Reference] | Setting/Method | Results and Conclusion | Comments |
|---|---|---|---|
| Retrospective [4] | The telephonic interview/By using 15 predefined premonitory symptoms questionnaire. | Prodromes are frequently reported by children and adolescents. Face changes seems peculiar to pediatric migraine. | This is only pediatric study. Hence, the results were compared with the adults. |
| Retrospective [5] | A clinic based population/A questionnaire study | Premonitory symptoms are frequently reported in migraine patients. Majority of these patients have atleast one symptom. | There was an overlap between prodromes and stress triggers. Because of female dominance (80%), selection bias is possible. |
| Prospective [6] | By general practitioners/A questionnaire study | Prodromes were more common in patients with aura and less frequent in patients on preventable medication. The most common individual true premonitory symptom was anxiety. | The study looked at premonitory and post ictal symptoms as well. |
| Prospective [7] | Outpatient Clinic/NA | A majority of patients had prodromes. The study emphasizes the importance of preventing the headache phase of acute migraine attack. | The study population included patients with or without aura. |
| Prospective [8] | At home/A three month electronic diary study | The study revealed that patients with migraine, who can report premonitory symptoms, can accurately predict a full blown headache. | The study demonstrated that prodromes are followed by a migraine attach in 72 hours in most of the patients. |
| Unclear [9] | Outpatient neurology or in general hospitals/By spontaneous or by direct questioning | Out of 50, 17 (34%) patients had symptoms that preceded headache for several hours. | Study provided a fundamental separation of headache phase of migraine from prodromes and aura. |
| Prospective [10] | Outpatient Headache Clinic/Clinical investigation | A family history of migraine,Onset of age was lower, and Incidence of triggers was higher in patients with prodrome. | The patients with prodromes and a family history of migraine are predisposed to migraine. |
| Retrospective [11] | Outpatient Clinic/Observational study | A large percentage of study population had atleast one premonitory symptom. | Only patients with documented prodromes were included. |
Our search revealed a single article in children with prodrome. The rest of the studies reported prevalence of prodromes in adults except one study which was carried out to separate migraine’ prodromes from aura and ictal phase [9].
Table 1: Summarizes the studies of prodrome performed in children and adults with migraine with and without aura [4-11].
Prevalence
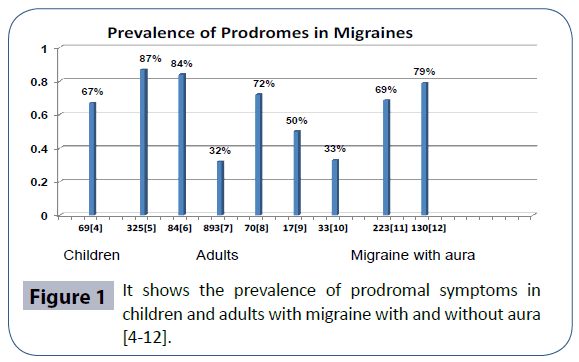
The prevalence of prodromes in migraines is shown in the Figure 1. In contrast to the adults, a lower prevalence of 67% was reported in children [4]. The cause for such a low prevalence is unknown. This difference may be due to a child’s inability to realize and verbalize or the way we elicit the symptom.
In an effort to improve accuracy of the prevalence of prodromes, the studies have included increasing numbers of predefined symptoms in clinic-based populations [4,5]. It should be noted that 121/164 (73.8%) patients with classical migraine had concurrent or past history of migraine without aura [12].
Overall the reporting of prevalence has improved from 12%- 79% to 67%-87% [13,14]. In part, this variability may reflect the variability in the symptomatology of preictal phase. To reduce such variability, the methodology to be used for assessing the prodromal symptoms should be considered carefully [15].
Additionally inclusion of preictal physical sign together with symptoms is likely to identify an impending ictal phase of migraine attack.
Clinical Characteristics of Prodrome
The reported clinical characteristics of prodrome in migraines and aura are shown in the Table 2.
| Study Reference | No. Patients | Mean Age Yr. (range) | Femalen (%) | Migraine Subtypes | Three Most CommonPremonitory Symptom or Comment | ||
|---|---|---|---|---|---|---|---|
| Without Aura n (%) | With Auran (%) | ||||||
| [4] a | 103 | 12.1 (5-16) |
46 (45) |
69 (67) |
11 (11) |
Facial pallor, Shadow under the eyes, and irritability | |
| [5] | 374 | 50 (30-50) |
300 (80) |
179 (48) |
195 (52) b |
Fatigue, Phonophobia,Yawning | |
| [6] | 100 | 39.3 (15-65) |
82 (82) |
85 (85) |
15 (15) |
Neuropsychiatric, 65% Sensory, 63% General and Digestive system 58% |
|
| [7] | 893 | 37.6 (13-80.5) |
760 (85.1) |
IHS 1.1-1.6 c IHS 1.1-1.7 c |
Tiredness, general malaise and Fatigue | ||
| [8] d | 97e | 42 (24-69) |
92 (95) | 72 (75) | NA | Tiredness, Difficulty to concentrate , and Stiffness of neck |
|
| [9] | 50 | 34 (12-59) |
28 | 31 | 15 g | Patients with undocumented prodromes were excluded. This might lead to selection bias. | |
| [10] | 100 | 41 (NA) |
76 (76%) | 100 | NA | Changes in mood, Sensory and psychophysical symptoms |
|
| [11] | 325 | 36.8 (NA) |
248 (76) |
NAp | 325 (6.7) f |
Positive and negative visual prodromes e |
|
| [12] | 164 | 30 (7-75) |
113 (68.9) |
NAp | 164 (100) |
79% Scintillating scotoma, 30% Paresthesias, and 18% Aphasic disturbances | |
a 23 children (22%) in the study had both migraine with and without aura;
b 195 (52%) an unusually high number of the patients with migraine with aura in the study;
c All 893 patients were diagnosed based on International Headache Society (IHS), 1988 from 1.1-1.7. The study did not breakdown into the migraine subtypes.
d The study excluded 23 patients with less than 3 attacks;
e Visual positive prodromes included; flashes, lights, fortification, scintillations, silver dots, streaks, wavy lines. The negative visual phenomena included hemianopia, scotoma, or blind spots
f It was unclear, if the subjects were migraine or general patient
g The study includes 3 hemiplegic and 1 patient with basilar migraine Most studies patients had migraine with and without aura. Only three studies reported prodromal mean symptoms 1.8, 3.2, and 6.8 per patients [4-6], respectively. Santoro’s studied exclusively common migraine [10]. Bana’s and Manzoni’s studied exclusively adult patients with classical migraine [11,12].
Table 2: Lists the clinical characteristics of prodrome in migraine with and without aura [4-12].
Symptomatology
Like subsequent phases of migraine, prodromal symptomatology is variable. The constellation of symptoms includes sensory, psychosomatic, autonomic, and motor dysfunctions. This variability in symptomatology occurs not only in different patients but also in two attacks of the same patient with migraine. Such a variable symptom of unknown etiology characterizes the preictal phase of migraine.
The prodromes can be a positive or negative neurologic sign or symptom. These symptoms include disturbances of mood such as irritability, restlessness, fatigue, tiredness, inattention, and rarely, hyperactivity. Anorexia and craving for food, salt, or sweet may be present. Excessive yawning for several hours preceding a headache is not unusual. Hypersensitivity to light (photophobia), sound (phonophobia), or odors (osmophobia) may occur as prodromal symptoms. They can occur several hours or even days prior to the ictal phase of migraine attacks [16].
Three most common prodromal symptoms are shown in the last column of the Table 2. Among pediatric migraine, the facial pallor, shadow under the eyes, and irritability are common. In adults, fatigue, tiredness, and psychosomatic symptoms were amongst the most common symptoms. Visual symptoms, both positive and negative, in migraine with aura were consistently different from those with migraine without aura.
Onset
The onset of prodromal symptoms is spontaneous. They usually occur in the early morning hours. However, the patient may not realize this until later in the day. Using an electronic diary, the migraineurs who reported prodromes can accurately predict the full-blown headache phase 72%.
Course
After onset, the course of the symptomatology builds-up. A shorter duration of prodromal builds-up is common in children. The prodromal symptoms maximize in its intensity during the ictal phase. Ictal phase is dominated by headache in migraine with and without aura or any neurological symptom other than headache in migraine–related conditions. The crescendo of prodromes can be fast, slow, and prolonged. This may have an undulating course in children with chronic daily headache of the migraine type.
Appearance and disappearance of prodromal symptoms were studied prospectively in 100 migraineurs. Both phases were experienced by 84% and 80% patients, respectively. The symptoms were also present in migraine with aura. The severity of headache was associated with a higher frequency of postictal symptoms. The patients who were on preventative medication had decreased frequency of future prodrome and to a lesser degree of postictal symptoms.
It should be noted that the prodromal phase is not limited to the very first phase of migraine. Its course is like a “Bell curve” along with variable type, severity, and duration of the symptomatology.
Postictal symptom: A few studies have explored postictal symptoms in migraines. Like the prodromal phase, the postictal phase is also gradual, but unlike prodromal phase, it is a receding phase of migraine. The most common postictal symptoms are physical and mental fatigue, depressed mood, inattention, reduced physical activities, and yawning. The number of symptoms ranged from 2 to 11 (average 6) per patient lasting for a mean of 18 hours. The range of symptoms beyond the ictal phase supports the notion that the entire brain is involved in migraine attacks [17]. A daily use of analgesic beyond three consecutive days can prolong the postictal phase of migraine.
Trigger factors
The triggers of migraine attack should be differentiated from risk factors, symptomatology of the prodromes, and side-effects of anti-migrainous medication.
The major risk factors for migraines are female sex and positive family history. However, a migraine attack is precipitated by “stress” [18], or change in patients’ daily lifestyle. The change could be in the external environment [19] or in the internal environment. The most important internal changes are sleep deprivation and missing a meal. Change in hormonal status during menstruation cycle is known to precipitate a migraine attack [20]. The same internal factors trigger migraine attacks in children. However, when asked what triggers their migraine, the usual answer is “I do not know.” Some patients are unable to make a temporal association between trigger factor and the attack of migraine.
Often, there is a tendency to report prodromal symptoms such as dizziness or worsening of symptoms on physical activity as the trigger for migraines. They are infrequently reported as the sideeffect of the preventive drug in use.
The clinically differentiating characteristics of visual symptoms in migraine and pseudo-tumor cerebri are shown in the Table 3.
| Symptoms of/Signifies | Characteristics | Clinical Diagnosis is made by |
|---|---|---|
| Prodrome/Migraine with and without aura | Blurry vision photophobia | Examining the rest of the migraine attack profile |
| Aura (convention)/Migraine with aura | Positive visual aura | Emergence of headache phase |
| Aura (non-convention)/Complicated migraine | Other than typical visual aura | Lack of prodrome or headache |
| Visual illusion/Alice in Wonderland syndrome | Transient episode of visual illusions include size, shape, color, movement, and time | Include micropsia (69%), teleopsia (50%), macropsia (25%), metamorphopsia (15%), and pelopsia (10%) |
| Visual obscurations/Pseudotumorcerebri | Transient episodic vision loss in the presence of persistent and prolonged headache in obese adolescence female | An increased intracranial opening pressure measured in calm patient with straight leg position |
Table 3: It shows the concise clinical characteristics of visual symptoms in migraines and pseudotumor cerebri.
Clinical Characteristics of Aura
The concept of aura in migraine came from epileptic events. The presence of visual aura and rarely cutaneous sensation, also known as typical or conventional aura, characterizes migraine with aura. The type of aura and its temporal relationship with the next evolving symptom during attack differentiate between subgroups of migraine [21]. Aura in migraine serves as a boundary between “migraine without aura” and “migraine with aura” [22] and “migraine-related condition.”
Charles reported that “Careful recording and analysis of visual aura symptoms provide new insight into the initiation and propagation of the underlying brain phenomenon” [23].
Typical or conventional aura
The typical aura of migraine includes visual aura. This does not include visual illusion which is the characteristic feature of Alice in Wonderland syndrome. A relatively short duration and termination of visual symptomatology before the onset of ictal phase characterize typical aura in migraine with aura. A free of symptoms interval between the end of visual aura and the beginning of headache has also been reported. This interval usually lasts less than an hour. In a retrospective study of twenty five migraineurs, three patients had normal healthy status and twenty-two patients (88%) had multiple symptoms consistent with a diffuse cerebral disturbance [24].
The symptoms of visual aura include photopsia or flashing lights, but this may take any form. Fortification spectrum is the term used to describe the bright zigzag lines. Some persons will have a loss of vision either as a blind spot (scotoma) or hemianopsia. Distorted or wavy vision is not uncommon. The typical visual aura starts as a small object and gradually enlarges or moves across the visual fields before disappearing. The visual disturbances in typical aura are not fixed or static. Bright colors are being seen commonly rather than dark or dim spots. They usually last 15 to 60 minutes. Most importantly, typical aura maintains the temporal relationship with prodrome and the ictal phase as described above.
Paraesthesias involving the limbs are probably the second most common aura in migraine. This should not be confused with allodynia of migraine. The tingling typically spreads slowly up or down in a hemiparetic pattern. It may affect the same side of the body, e.g. the leg, arm, face, or tongue. A slowly spreading tingling over several minutes is an important characteristic that differentiates migraine with aura from the sudden onset paresthesia that occurs in transient ischemic attacks. Basilar type migraine involves diplegic pattern of paresthesia. Motor dysfunctions such as cortical weakness although rare do occur in children with hemiplegic migraine.
Atypical paresthesia in character or course should prompt investigation for conditions like arteriovenous malformation or mesial temporal sclerosis [25].
Atypical or non-conventional aura
Migraine-related condition is characterized by the presence of atypical or non-conventional aura, which includes non-visual aura. This occurs in the presence of insignificant prodromal symptoms. Atypical aura does not respect the boundaries of the three phases of migraine attack profile. In fact, they may continue well beyond the ictal phase. They may last for several hours, days, or even weeks.
The symptoms of atypical aura include visual illusion, atypical cutaneous sensation, vestibular, auditory, or motor dysfunction. Metamorphopsia, in which objects appear larger or smaller than they actually are, characterizes Alice in Wonderland syndrome. Ringing in ear, auditory hallucination, and sudden hearing loss are uncommon [26-28], but they can present in isolation or cooccur with migraine. In the presence of atypical aura, a diagnosis of migraine like syndromes should be explored.
Migraine–related conditions can be differentiated from other types of migraine by an abrupt onset of a dominant symptom other than headache in the absence of an alternative explanation [29,30].
The differential diagnosis of prodrome and aura of migraine, and epilepsy are shown in the Table 4.
| Prodromes ofMigraines | Conditions | Epileptic Aura [31] | ||
|---|---|---|---|---|
| Migraine with aura | Migraine-related | |||
| Onset | A gradual building- up before ictal phase onset of migraine | Acute or subacute onset | Acute or subacute | Sudden |
| Presentation | A variable combination of positive or negative neurologic sing or symptom. | Usually positive symptomatology like visual or somatosensory cutaneous symptoms [27] | Transient neurologic sign or symptom other than headache | Likely stereotypic a Positive symptoms, Commonly epigastric pain or fear or vertigo |
| Relationships | Submerged with the ictal phase of migraine with or without aura | Starts and terminates before onset of ictal phase | Starts but it does not terminate before ictal phase | Just before ictal phase of the event |
| Duration | 2-48 hours before ictal phase of migraine | 20 minutes to 2 hours | Hours, days , or weeks | 5 minutes to 30 minutes |
| Course | A Bell shape course ; an initial crescendo course, maximizes in middle and then recedes, resolves in post ictal phase | Relatively faster and it has a relatively shorter course than the prodromes | Continue through the entire ictal and postictal phases | Faster and of short duration than the aura of migraine |
| Resolves | Slowly recedes and resolves in postictal phase of migraine with or without aura | Before onset of the ictal phase | Long after resolution of other symptoms of postictal phase | Probably at start of ictal phase |
| Remark | When present, this is followed by a migraine attack within 72 hours on 72% of occasions. | Patient may not volunteer the symptoms of the prodromes. | Prodromes may be present but in the presence of a vivid aura it may be overlooked. | Pathophysiologically, epileptic aura is the result of a functional cortical zone activation |
Table 4: It summarizes differential diagnosis of prodrome and aura of migraine, and epilepsy.
Diagnostic Challenge
There are several challenges in making a clinical diagnosis of migraines:
(1) The ICHD-III diagnostic criteria do not acknowledge the importance of prodromal symptoms in migraine.
(2) There is no diagnostic biomarker for migraines.
(3) The patient may not be aware of their symptoms or their temporal relationship with migraine.
(4) Some physicians may not have appreciated yet the variability or atypical aura in migraine.
(5) The history is gathered based on a fixed-set of predetermined questions and of adults’ symptomatology. These methods do not allow the parents to express additional concerns and do not encompass symptomatology pertaining to children, which are unlikely to capture the entire prodromal manifestation.
(6) The presence of mimicking conditions like epileptic aura or aura of encephalitis may further complicate the clinical diagnosis.
Epileptic aura
In contrast to migraine, epileptic prodrome is relatively rare. A Hungarian multicenter study assessed the frequency of the warning symptoms preceding an epileptic seizure. In five hundred and sixty two patients, out of total 1,124, with epilepsy, about 50% experienced warning symptoms before their seizures. The symptoms included epigastric sensation, dysphoria, and headache. Epileptological data revealed that warning symptoms occur primarily in focal and complex partial seizures [31].
Alving’s studied EEG changes during epileptic prodromes. Ten out of four hundred ninety (2%) patients had prodromes. During prodrome, the EEG was recorded in 6 patients. The EEG in 3 patients correlated with non-convulsive status epilepticus. In other 3 patients, EEG revealed no abnormalities. The author of the study concluded that the epileptic prodromes should be treated as nonconvulsive status epilepticus of ictal phenomena [32]. Both, migraine and epilepsy are closely related disorders. But they have their own distinct distinguishing characters [33].
The temporal association between epileptic seizures and headache attacks has created controversial terminologies. The International Classification of Headache Disorders-2 defines three types of association:
(1) Migraine-triggered seizure
(2) Hemicrania epileptic
(3) Post-ictal headache, unlike migraine, postictal symptom can be a presenting manifestation of a seizure [34].
Encephalitis
The manifestation of encephalitis may mimic prodromes of migraine [35]. However, the constellation of an acute onset, a rapidly worsening short course of a vivid symptomatology can differentiate the prodrome of encephalitis from migraine. In addition to other procedures, the performance of an urgent magnetic resonance imaging (MRI) of the brain is indicated to confirm the clinical diagnosis of encephalitis [36].
This clinical distinction diminishes in patients with migrainelike syndromes. Recently, a 15-year-old female whose initial presentation was thought to be the manifestation of migraine, however, an MRI of the brain revealed a diagnosis of acute disseminated encephalomyelitis. A second condition in patient with migraine is rare. But this could be identified clinically by examining the clinical profile of migraine and migraine-like syndrome independently.
Prodrome of cluster headache
Cluster headache, another primary headache, is rare in children. But this is the most common disorder of trigeminal autonomic cephalgias. It is characterized by unilateral headache with predominant ipsilateral autonomic symptoms such as sneezing, nasal congestion, pink conjunctiva, and excessive tears [37].
Clinical profile of cluster headache is very distinct and is the opposite of migraine. For example, migraine is common and cluster headache is rare. Migraine is common in female and cluster headache is common in males. Migraine attacks predominantly occur upon awakening in the morning or day time as compared to cluster headaches, which often occur during sleep.
However, some patients with cluster headache do have migrainous features [38]. Mood, cognition, and alimentary symptoms suggest a diffuse cerebral disturbance in both migraines and cluster headache, but onset of prodromal symptoms in cluster headache occurs for a period of several days, weeks, or even months [39].
Diagnostic and Therapeutic Significance
The diagnosis of migraine remains largely clinical. Eliciting the history, particularly in children, requires strategic questioning and a lot of patience. The way questions are worded can be the single most important clinical maneuver in making the diagnosis of migraines. The questions should be open ended with no suggestions. They should be directed to explore the migraine attack profile in relation to the timeline of evolving symptomatology.
Physical signs of prodrome in migraine
Almost all studies have emphasized the symptoms of prodromes. To elicit the physical signs of prodrome particularly in children the questions should be directed to the mother. A change of behavior such as irritability and pallor facial color are common.
Consideration of the observed physical signs is likely to increase the prevalence of prodromal symptomatology. Thus, it will increase the accuracy of clinical diagnosis of migraine in children.
Alternative diagnosis in migraine
Alternative diagnoses such as refractive errors, sinus disease, depression, and anxiety for migraines are a common occurrence. Migraine should be considered by examining closely the preictal symptoms of prodrome or aura in the context of other symptoms. Given a high prevalence of the migraines, uncommon presenting features of migraine are common. Thus, even a rare or unrecognized presentation should be considered in the differential diagnosis of migraine [40].
Therapeutic significance
Identification of preictal symptomatology of migraine is not only important for affirmative clinical diagnosis of migraine but also has a pivotal therapeutic implication. Recognition of preictal symptomatology provides an earliest opportunity for a therapeutic intervention. This minimizes the severity and duration of the individual attack of migraines.
Distinguishing the trigger factors from true symptomology of prodrome of migraine will allow patients:
(1) To make sure not to miss their meals
(2) To take analgesic promptly
(3) To drink ample of water
(4) To adapt to a less interactive physical and mental attitude for the rest of the day to avoid worsening of the migrainous symptoms.
The trigger factors are primarily managed by sleeping and eating on time which act to prevent future attacks of migraine. Frequently, the patients attribute prodromal symptoms such as dizziness or tiredness of migraine to a side-effect of the preventive drug in use. This is not an indication to discontinue the medication. Rather, this may require increasing the dose in those patients whose sleeping and eating pattern have been regular. The use of oral analgesic should be avoided during the receding postictal phase of migraine. This will prevent transformation of episodic migraine attacks to a chronic daily headache of the migraine type [41].
Future
Future study should explore the prodromal symptoms together with physical signs particularly in children. The trigger factors and spectrum of non-conventional aura should be explored. These findings should be statistically analyzed.
The diagnostic and therapeutic potentials of prodromes and trigger factors can be improved by selecting an appropriate methodology. To minimize the variability in reporting a “multimodal approach” has been recommended [42].
Additionally, acknowledgement of an appropriate status of prodrome of migraines in International Classification of Headache Disorders will play an active supportive role for the clinical diagnosis of the migraines.
Summary
The ictal symptomatology in adults with migraine in contrast to children has been well described. All studies in adults have emphasized preictal symptoms, while a single study performed in children emphasized “preictal sign” along with symptom. No information was available pertaining to the preictal phase of migraine-related condition.
The clinical characteristics of preictal symptoms and their relationship with various types of auras are unique. In lack of any alternative explanation, their clinical characteristics are sufficient in making an active clinical diagnosis of migraines. Notably, the presence of atypical aura and its continuation beyond postictal phase characterizes migraine–related conditions.
Accuracy of clinical diagnosis of various subtypes of migraines can be further increased by including prodromal physical signs together with symptoms and considering their temporal relationship with the rest of the migraine attack profile. This is best achieved by avoiding undue emphasis on the headache itself.
The prodromal symptomatology may be unrecognized particularly by young children. Awareness of preictal symptoms offers a diagnostic opportunity for clinicians and an earliest possible therapeutic window for patients. Most importantly, this provides patients with a sense of self-control and relief from the burden of migraine.
Acknowledgement
Authors thanks to Dawn M Fields for her sincere help in obtaining the full text of the needed articles.
Authors’ Contribution
Gira Borad searched, prepared the tables, contributed, and approved the final version.
Vikash S Gupta prepared initial version of the draft, contributed, and approved the final version.
Surya N Gupta initiated, supervised, coordinated, and contributed in discussion of migraine and prodromes, and approved the final version of this manuscript.
Conflict
None
References
- Gupta SN, Gupta VS (2014) Bilateral Tongue Bite during Epileptic Seizure: Nomenclature and Mechanism. Austin J NeurolDisord Epilepsy1: 1-2.
- Headache Classification Committee of the International Headache Society (IHS) (2013) The International Classification of Headache Disorders (3rd edn, beta version). Cephalalgia33:629-808.
- Gupta SN, Gupta VS, Fields DM (2015) Spectrum of complicated migraine in children: A common profile in aid to clinical diagnosis. World J ClinPediatr 4: 1-12.
- Cuvellier JC, Mars A, Vallee L (2009) The prevalence of premonitory symptoms in paediatric migraine: a questionnaire study in 103 children and adolescents. Cephalalgia 29: 1197-1201.
- Schoonman GG, Evers DJ, Terwindt GM, van Dijk JG, Ferrari MD (2006) The prevalence of premonitory symptoms in migraine: a questionnaire study in 461 patients. Cephalalgia 26: 1209-1213.
- Quintela E, Castillo J, Munoz P, Pascual J (2006) Premonitory and resolution symptoms in migraine: a prospective study in 100 unselected patients. Cephalalgia 26: 1051-1060.
- Kelman L (2004) The premonitory symptoms (prodrome): a tertiary care study of 893 migraineurs. Headache 44: 865-872.
- Giffin NJ, Ruggiero L, Lipton RB, Silberstein SD, Tvedskov JF, et al. (2003) Premonitory symptoms in migraine: an electronic diary study. Neurology 60: 935-940.
- Blau JN (1980) Migraine prodromes separated from the aura: complete migraine. Br Med J 281: 658-660.
- Santoro G,Bernasconi F, Sessa F, Venco A (1990) Premonitory symptoms in migraine without aura: a clinical investigation. FunctNeurol 5: 339-344.
- Bana DS, Graham JR (1986) Observations on prodromes of classic migraine in a headache clinic population. Headache 26: 216-219.
- Manzoni GC, Farina S, Lanfranchi M, Solari A (1985) Classic migraine-clinical findings in 164 patients. EurNeurol 24: 163-169.
- Rasmussen BK,Olesen J (1992) Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia 12: 221-228.
- Amery WK, Waelkens J, Vandenbergh V (1986) Migraine warnings. Headache 26: 60-66.
- Lipton RB,Pavlovic JM, Haut SR, Grosberg BM, Buse DC (2014) Methodological issues in studying trigger factors and premonitory features of migraine. Headache 54: 1661-1669.
- Kunkel RS (2001) Clinical manifestations of migraine. Clin Cornerstone 4: 18-25.
- Blau JN (1991) Migraine postdromes: symptoms after attacks. Cephalalgia 11: 229-231.
- Baldacci F,Vedovello M, Ulivi M, Vergallo A, Poletti M, et al. (2013) How aware are migraineurs of their triggers? Headache 53: 834-837.
- Fraga MD,Pinho RS, Andreoni S, Vitalle MS, Fisberg M, et al. (2013) Trigger factors mainly from the environmental type are reported by adolescents with migraine. ArqNeuropsiquiatr 71: 290-293.
- Parashar R,Bhalla P, Rai NK, Pakhare A, Babbar R (2014) Migraine: is it related to hormonal disturbances or stress? Int J Womens Health 6: 921-925.
- Petrusic I,Pavlovski V, Vucinic D, Jancic J (2014) Features of migraine aura in teenagers. J Headache Pain 15: 87.
- Lardreau E (2007) The difference between epileptic auras and migrainous auras in the 19th century. Cephalalgia 27: 1378-1385.
- Charles A, Hansen JM (2015) Migraine aura: new ideas about cause, classification, and clinical significance. CurrOpinNeurol 28: 255-260.
- Blau JN (1992) Classical migraine: symptoms between visual aura and headache onset. Lancet 340: 355-356.
- Erickson JC, Clapp LE, Ford G, Jabbari B (2006) Somatosensory auras in refractory temporal lobe epilepsy. Epilepsia 47: 202-206.
- Miller EE, Grosberg BM, Crystal SC, Robbins MS (2015) Auditory hallucinations associated with migraine: Case series and literature review. Cephalalgia 35: 923-930.
- Viirre ES,Baloh RW (1996) Migraine as a cause of sudden hearing loss. Headache 36: 24-28.
- Smith RA, Wright B, Bennett S (2015) Hallucinations and illusions in migraine in children and the Alice in Wonderland Syndrome. Arch Dis Child 100: 296-298.
- Gupta SN, Gupta VS, Borad N (2016) Spectrum of migraine variants and beyond: The individual syndromes in children. Brain Dev 38: 10-26.
- Rothner AD, Parikh S (2016) Migraine Variants or Episodic Syndromes That May Be Associated With Migraine and Other Unusual Pediatric Headache Syndromes. Headache 56: 206-214.
- Rajna P, Clemens B, Csibri E, Dobos E, Geregely A, et al. (1997) Hungarian multicentre epidemiologic study of the warning and initial symptoms (prodrome, aura) of epileptic seizures. Seizure 6: 361-368.
- Alving J,Beniczky S (2013) Epileptic prodromes: are they non-convulsive status epilepticus? Seizure 22: 522-527.
- Cianchetti C,Pruna D, Ledda M (2013) Epileptic seizures and headache/migraine: a review of types of association and terminology. Seizure 22: 679-685.
- Nye BL,Thadani VM (2015) Migraine and epilepsy: review of the literature. Headache 55: 359-380.
- Kravljanac R, Djuric M (2012) [Childhood epileptic seizures imitating migraine and encephalitis]. SrpArhCelokLek 140: 558-562.
- Chow FC, Glaser CA, Sheriff H, Xia D, Messenger S, et al. (2015) Use of clinical and neuroimaging characteristics to distinguish temporal lobe herpes simplex encephalitis from its mimics. Clin Infect Dis 60: 1377-1383.
- Horven I, Sjaastad O (1977) Cluster headache syndrome and migrain. Ophthalmological support for a two-entity theory. ActaOphthalmol (Copenh) 55: 35-51.
- Matharu MS,Goadsby PJ (2002) Trigeminal autonomic cephalgias. J NeurolNeurosurg Psychiatry 72 Suppl 2: ii19-19ii26.
- Blau JN, Engel HO (1998) Premonitory and prodromal symptoms in cluster headache. Cephalalgia 18: 91-93.
- Angus-Leppan H (2013) Migraine: mimics, borderlands and chameleons. PractNeurol 13: 308-318.
- Kacperski J (2015) Prophylaxis of migraine in children and adolescents. Paediatr Drugs 17: 217-226.
- Pavlovic JM,Buse DC, Sollars CM, Haut S, Lipton RB (2014) Trigger factors and premonitory features of migraine attacks: summary of studies . Headache 54: 1670-1679.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences