Two Needle Electrode System for Trigeminal Neuralgia Radiofrequency of Gasserian Ganglion
Escosa Bae M
DOI10.4172/2472-1913.100035
Escosa Bae M*
Department of Neurosciences, King Faisal Specialist Hospital and Research Center, Jeddah, Kingdom of Saudi Arabia
- *Corresponding Author:
- Escosa Bae M
Department of Neurosciences
King Faisal Specialist Hospital and Research Center
Jeddah, Kingdom of Saudi Arabia
Tel: 977 29 58 00
E-mail: mark.escosa55@gmail.com
Received Date: March 28, 2017; Accepted Date: April 25, 2017; Published Date: May 05, 2017
Citation: Escosa Bae M. Two Needle Electrode System for Trigeminal Neuralgia Radiofrequency of Gasserian Ganglion. J Headache Pain Manag. 2017, 2:1. doi: 10.4172/2472-1913.100035
Abstract
Radiofrequency (RF) is one of the most common procedures used to treat trigeminal neuralgia (TN). Ophthalmic division (V1) is the most distant division to reach with the needle electrode and probably the most difficult to treat with RF. In an attempt to improve results and reduce complications in treating TN involving V1 we propose an operative procedure using two needles method for continuous RF (CRF) of Gasserian ganglion (GG). A total of 63 patients with idiopathic trigeminal neuralgia (ITN) were selected from 2011 to 2017 to treat with this method and were followed-up for one year. During this period of time 90% of patients were completely pain free after the procedure, no major complications were found and no pain recurrence was observed.
Keywords
Trigeminal neuralgia; Gasserian ganglion; Radiofrequency
Introduction
Treatment of TN with RF when V1 division is affected is controversial, with few works explaining results [1,2]. Rates of complications and pain recurrence are reported higher than other divisions of the nerve [2]. CRF is reported to give higher rates of complete pain relief than either stereotactic radio surgery or glycerol rhizolysis [3,4]. The procedure success rate of RFT approaches 100%, being superior to that of Microvascular Decompression (MVD), which is only 85%. However, its long-term efficacy is lower [4], with the advantage that it can be repeated, if required [5].
Taha and Tew [4] have proposed that neurosurgeons should gain proficiency in different techniques, so as to be able to offer the most suitable procedure for individual patients. MVD is better recommended for healthy patients with isolated pain in the distribution of the first division or of all 3 divisions of the trigeminal nerve, and in patients who refuse sensory deficit. However, effective rate of different branches on ITN is poorly known [4,6].
Most of the pain in ITN happens in V2 or V3 and only 5% of pain is in V1 [7,8]. CRF of V1 has been controversial and challenging due to the ophthalmic division fibers transmitting corneal sensations and can easily induce inflammation, and corneal ulcers. Huang and Liu [1], studied the results of V1 CRF demonstrating that is effective and safe. These results are the basis for investigating and arguing new methods to improve results related with RF treatment.
Anatomically, V1 leaves GG through the superior part in the Meckel’s cave and carries sensory information and sympathetic fibers for pupil dilation [9]. V1 Is the most distant division to reach with the needle and probably the more difficult to treat with the usual one needle electrode RF.
In this article, we propose and describe the two needle CRF of GG procedure for TN, in an attempt to improve results and evaluate risks in treating TN when V1 is involved. The usual one needle procedure has a high rate of pain recurrence. We propose the explanation that two needles can reach more than one division during RF. Results and safeness are discussed.
Materials and Methods
Patients eligible for the procedure were previously diagnosed of ITN using the criteria of the International Classification of Headache Disorders-II (intense paroxysmal attacks, lasting seconds to two minutes that can be precipitated by trigger factors without neurological deficit and no attributed to another disorder). RF was generally offered to patients who fail medical treatment, have only partial relief of pain after 1 year or have developed complications or side effects of medical management and either have already had or are not suitable candidates for MVD. All patients received a cranial Magnetic Resonance Imaging (MRI) to exclude other causes of TN before the procedure. The follow-up information on patients was done during the first year every two months checking pain relief, recurrence and complication rates.
A total of 63 patients with pain affecting at least V1 were studied in Joan XXIII University Hospital, Spain, between the years 2011 and 2017. Patients with severe cerebrovascular, cranial tumors or cardiovascular disease were excluded. Cranial nerves were explored before and after the procedure and a Schirmer's test was performed also in all patients before and after the procedure. Patients with other problems like skin infection or coagulopathies were carefully selected to avoid complications related with the procedure.
When Isolated V1 involvement was found (occurs in less than 5% of TN patients) additional work-up to rule out other conditions such as temporal arteritis, herpes zoster, ocular migraine, paroxysmal hemicranias, cluster headache syndrome, short-lasting unilateral neuralgiform headaches with conjunctival injection and tearing, or short-lasting unilateral neuralgiform headaches with cranial autonomic symptoms.
Patients are advised that, although most percutaneous procedures can be performed as day surgery, they may be required to stay overnight in the hospital if circumstances dictate. Anticoagulant and antiplatelet medications should be stopped before surgery, and patients are advised to continue taking any antihypertensive medications throughout the perioperative period. Patients are advised to take nothing by mouth on the day of the procedure.
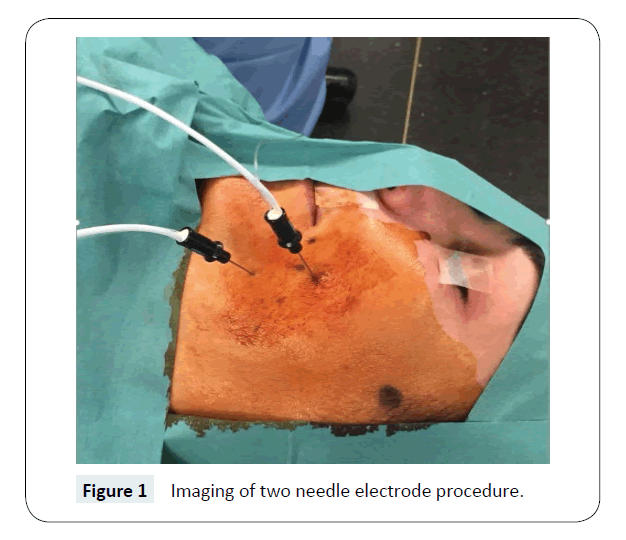
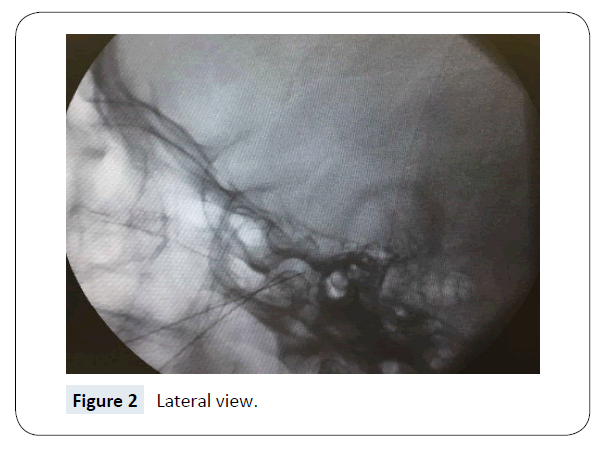
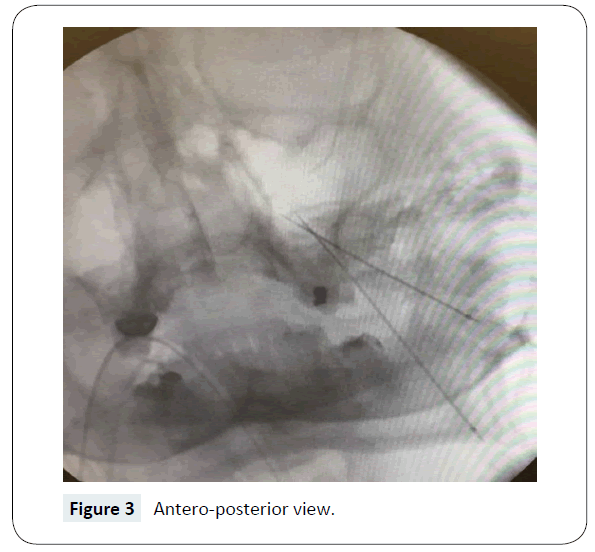
The procedure was undertaken under general anesthesia performed by a single surgeon. Operative technique involved freehand cannulation using Hartel landmarks [7] with a variation in the occlusal plane insertion. The first needle is inserted into the cheek at a point 2.5 cm from the corner of the mouth, 1 cm below the occlusal plane. The second one is inserted into the cheek at a point 2.5 cm from the corner of the mouth, 1 cm above the occlusal plane (Figure 1). Location within the foramen ovale and trigeminal cistern was confirmed with the image intensifier in the lateral plane and in the needle guidance view (Figures 2 and 3).
A receding tract of multiple lesions (4–5 in total at 5-mm intervals, as is the electrode tip) at 65°C for 90 seconds was performed in each needle, one after the other, at the same plane.
Outcome criteria included pain relief, recurrence adverse events as documented in the post-op consultant clinic review.
Pain relief was defined as: total (no pain off medication); partial (improved pain but still requiring medication); no benefit; dysaesthetic pain or anesthesia dolorosa.
Ethics committee was consulted. Proper explanation of different treatment options, risks and informed consent were obtained in all patients.
The statistical analysis for this retrospective study was performed using SPSS Ver. 20.0 (SPSS Inc., Chicago, IL, USA). Quantitative data were expressed as median, standard deviation and range in this descriptive analysis.
Results
We studied retrospectively 63 patients from 26 to 92 years old, 61% Females and 39% males. Pain distribution was more usual in all the branches (71%), followed by V1 (16%) and V1+V2 (9%) and both sides were similar (45% vs. 55%) (Table 1).
| No. of patients | 63 |
|---|---|
| Age (years, mean, minimum-maximum) | 65 (26-92) |
| Gender (female/male) | 61%/39% |
| Preoperative duration of symptoms (mean ± SD, years) | 6.2 ± 4.7 |
| Postoperative follow-up (mean ± SD, years) | 1 ± 0.2 |
| Right Side affected | 45% |
| Left Side affected | 55% |
| V1 | 16% |
| V1+V2 | 9% |
| V1+V3 | 4% |
| V1+V2+V3 | 71% |
Table 1: Clinical data (SD: Standard Deviation).
Pain was completely relieved in more than 90% for all the different combination of pain distribution (Table 2). Facial hematoma was found in 9%, mouth penetration 4%, facial numbness was the most frequent complication with 19%, corneal hypoesthesia 16% (Schirmer's test was positive in these cases), severe dysesthesia 6% and transient motor weakness 12% (Table 3).
| Branch | No pain, no medication | Residual pain, with medication |
|---|---|---|
| V1 | 95% | 5% |
| V1+V2 | 95% | 5% |
| V1+V3 | 93% | 7% |
| V1+V2+V3 | 91% | 9% |
Table 2: Pain relieved in the first year.
| Facial hematoma | 9% |
| Mouth penetration | 4% |
| Facial numbness | 19% |
| Corneal hypoesthesia and reflex | 16% |
| Severe dysesthesia | 6% |
| Transient motor weakness | 12% |
Table 3: Complications.
Discussion
CRF for TN has shown to be effective in treating the maxillary (V2) and mandibular (V3) divisions, but the efficacy and safety of the ophthalmic division (V1) has been controversial. Recently Huang et al. [1], it was discovered that V1 RF in GG at 60–66°C can relieve TN immediately and can maintain the corneal reflex in most patients with a low complication rate. The recurrence rate of V1 TN has been reported in 22-65% with 65-75°C [6,10-12].
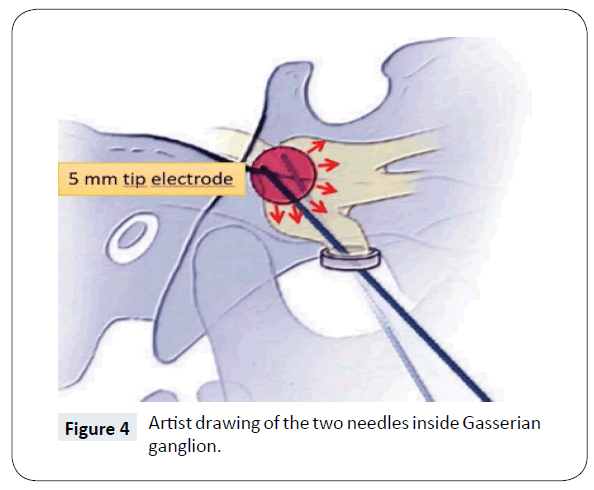
One of our objectives was to improve these previous results with our two needle CRF of GG procedure for TN, being a variant of the usual one needle procedure with the proposed explanation that can be more effective for patients with pain involving at least V1. With two needles electrode, the amount of tissue inside the GG heated up to 65°C is expected to be much more effective for the pain management than previously reported (Figure 4). We used the same technique and the same surgeon in all the patients to avoid misinterpretation of the results, obtaining completely relieved in more than 90% for all the different combination of pain distribution (only one patient had a corneal ulcer).
Previous studies report pain free rates during first year after RF between 68-85% [13,14]. Kanpolat et al. [15], finds a recurrence rate of 7.7% in the first 6 months after RF and 17.4% later on.
We achieved 90% in the first year, providing better results than before. Our procedure demonstrates that with two needles the treatment is more effective due to the amount of tissue inside GG heated with RF.
The underlying mechanism of RF for effectively relieving the neuropathic pain by higher temperatures was due to damaging the nerve’s pain signal transmission, as well as nonmyelinated fibers that conduct epicritic stimuli and block the transmission of electric activity [8]. In our study although there are 16% of patients that suffer from a decreased corneal reflex, only one patient had a corneal ulcer with good evolution. We used a temperature of 65°C for all the patients being well tolerated and safe. It’s well-known that serious complications often occur at a temperature ≥70°C [16-18]. Our opinion is that the optimal temperature should be between 60 and 65°C. We found Schirmer's test a good indicator after the procedure for using artificial tears to prevent corneal ulcers.
Seldom specialized published study reports on RF only for V1 branch TN. Efficacy and complications of RF for V1 TN are difficult to deduce from those studies. In addition, information on temperature used for CRF for V1 TN was not mentioned in some reports [19,20]. Using previous reports information [1,12,17- 18] we adjusted the temperature to less than 70°C and all the procedure was performed under general anesthesia. Facial numbness was found the most frequent transient complication (19%) that improved in more than 50% after 2 months and almost 90% in 10 months. Severe dysesthesia (6%) and transient motor weakness (12%) were found to be similar as in other studies [21,22].
Although the procedure was effective in more than 90% of the patients, 10% had some residual pain and were recommended to continue medication. In the first postoperative days, pain relief was near 100% and all patients expressed important solace. During the follow up year 10% of patients showed some recurrence of pain that was well tolerated with medication. All these patients were offered to repeat the procedure but they preferred to wait maintaining medication.
As we only follow up for 1 year all the patients, we don't know how many patients will need a second procedure after that period of time. Another aspect of this work is the wide range of age in this sample of few patients. This makes it difficult to draw further conclusions related with different age ranges and effectiveness of the procedure in different groups. Another important limitation of the study is related with the comparison with other studies, due to the important variability observed in patient populations and results related with the different divisions of the trigeminal nerve. More long-term follow up studies are fully recommended.
Conclusion
The two-needle electrode system for idiopathic trigeminal neuralgia radiofrequency of Gasserian ganglion seems to be effective and safe when V1 division is involved. This procedure achieves better results in the postoperative time and during the first year follow up as compared with previous studies. More long-term follow up studies are fully recommended.
References
- Huang Q, Liu X, Chen J, Bao C (2016) The Effectiveness and Safety of Thermocoagulation Radiofrequency Treatment of the Ophthalmic Division (V1) and/or Maxillary (V2) and Mandibular (V3) Division in Idiopathic Trigeminal Neuralgia: An Observational Study. Pain Physician 19: E1041-E1047.
- Yao P, Hong T, Zhu YQ, Li HX, Wang ZB, et al. (2016) Efficacy and safety of continuous radiofrequency thermocoagulation plus pulsed radiofrequency for treatment of V1 trigeminal neuralgia: A prospective cohort study. Medicine (Baltimore) 95: e5247.
- Lopez BC, Hamlyn PJ, Zakrzewska JM (2004) Systematic review of ablative neurosurgical techniques for the treatment of trigeminal neuralgia. Neurosurgery 54: 973-982.
- Taha JM, Tew JJ (1996) Comparison of surgical treatments for trigeminal neuralgia: reevaluation of radiofrequency rhizotomy. Neurosurgery 38: 865-871.
- Tang YZ, Jin D, Li XY, Lai GH, Li N, et al. (2014) Repeated CT-guided percutaneous radiofrequency thermocoagulation for recurrent trigeminal neuralgia. Eur Neurol 72: 54-59.
- Tang YZ, Wu BS, Yang LQ (2015) The long-term effective rate of different branches of idiopathic trigeminal neuralgia after single radiofrequency thermocoagulation: a cohort study. Medicine (Baltimore) 94: e1994.
- Hartel F (1912) Block anaesthesia and infection of the Gasserian ganglion and the trigeminal roots. Langenbecks Arch Klin Chir 100: 16.
- Son BC, Kim HS, Kim IS, Yang SH, Lee SW (2011) Percutaneous radiofrequency thermocoagulation under fluoroscopic image-guidance for idiopathic trigeminal neuralgia. J Korean Neurosurg Soc 50: 446-452.
- Graff-Radford S, Gordon R, Ganal J, Tetradis S (2015) Trigeminal neuralgia and facial pain imaging. Curr Pain Headache Rep 19: 19.
- Xue T, Yang W, Guo Y (2015) 3D image-guided percutaneous radiofrequency thermocoagulation of the maxillary branch of the trigeminal nerve through foramen rotundum for the treatment of trigeminal neuralgia. Medicine (Baltimore) 94: e1954.
- Tatli M, Satici O, Kanpolat Y (2008) Various surgical modalities for trigeminal neuralgia: literature study of respective long-term outcomes. Acta Neurochirurgica 150: 243-255.
- Xu SJ, Zhang WH, Chen T (2006) Neuronavigator-guided percutaneous radiofrequency thermocoagulation in the treatment of intractable trigeminal neuralgia. Chin Med J (Engl) 119: 1528-1535.
- Obermann M (2010) Treatment options in trigeminal neuralgia. Ther Adv Neurol Disord 3: 107-115.
- Broggi G, Franzini A, Giorgi C (1993) Trigeminal neuralgia: new surgical strategies. Acta Neurochir Suppl (Wien) 58: 171-173.
- Kanpolat Y, Savas A, Bekar A (2001) Percutaneous controlled radiofrequency trigeminal rhizotomy for the treatment of idiopathic trigeminal neuralgia: 25-year experience with 1,600 patients. Neurosurgery 48: 524-532.
- Erdine S, Ozyalcin NS, Cimen A (2007) Comparison of pulsed radiofrequency with conventional thermocoagulation in the treatment of iopathic trigeminal neuralgia. Eur J Pain 11: 309-313.
- Fraioli MF, Cristino B, Moschettoni L (2009) Validity of percutaneous controlled radiofrequency thermocoagulation in the treatment of isolated third division trigeminal neuralgia. Surg Neurol 71: 180-183.
- Wael F (2011) Management of trigeminal neuralgia by radiofrequency thermocoagulation. Alexandria J Med 47: 79-86.
- Teixeira MJ, Siqueira SR, Almeida GM (2006) Percutaneous radiofrequency rhizotomy and neurovascular decompression of the trigeminal nerve for the treatment of facial pain. Arq Neuropsiquiatr 64: 983-989.
- Udupi BP, Chouhan RS, Dash HH (2012) Comparative evaluation of percutaneous retrogasserian glycerol rhizolysis and radiofrequency thermocoagulation techniques in the management of trigeminal neuralgia. Neurosurgery 70: 407-413.
- Taha JM, Tew JM (2000) Percutaneous rhizotomy in the treatment of intractable facial pain. In: Schmidek H (ed.) Schmidek and Sweet Operative Neurosurgical Techniques: Indications, Methods, and Results (4th edn.), W.B. Saunders, Philadelphia, pp: 1537-1551.
- Steiger H (1991) Prognostic factors in the treatment of trigeminal neuralgia: analysis of a differential therapeutic approach. Acta Neurochir (Wien) 113: 11-17.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences